Final ID: TAC269
Validating a Predictive Model for Postpartum Hypertension Readmission with Incorporation of Social Vulnerability Index
Abstract Body: Introduction Hypertensive disorders of pregnancy (HDP) are a common cause of postpartum (PP) readmission. Predicting who has a high likelihood of HDP readmission may help optimize discharge planning & mitigate readmission risk. Neighborhood-level social determinants of health (SDH) have been linked to higher PP readmission risk. A recently published calculator for HDP readmission did not include SDH variables. We sought to validate & enhance this prior model by incorporating a meaure of SDH.
Hypothesis Model performance after external validation of a predictive model for PP HDP readmission would be enhanced by adding neighborhood-level SDH.
Methods Retrospective cohort study of deliveries from 2019-2022 using data from two hospital systems in Texas. PP readmission included inpatient stays with a diagnostic code of HDP occurring 1-42 days post-delivery discharge. Census-tract level Social Vulnerability Index (SVI) score was obtained using residential address at delivery. Site-specific model validation & recalibration were performed; models were assessed with concordance statistics (c- statistic) & Akaike information criterion (AIC), comparing the original calculator to the recalibrated & refit models, & the refit model with & without SVI.
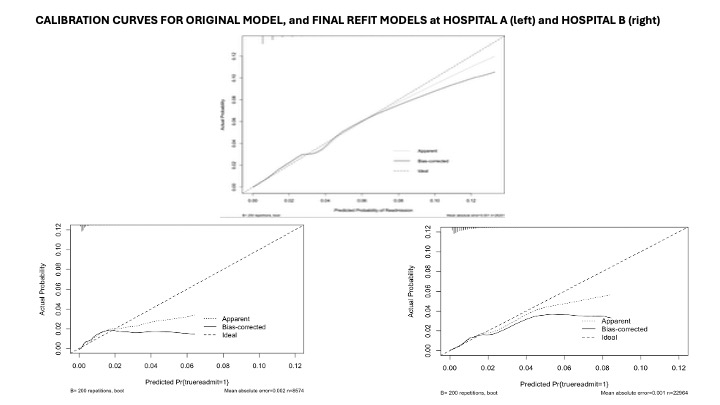
Results Readmission frequency at Hospital A was 0.5% (48 readmissions/8,646 deliveries) & at Hospital B was 0.7% (163 readmissions/22,966 deliveries). Median SVI score was 0.84 & 0.46 in Hospitals A & B. Model performance using the original calculator (c-statistic 0.80) was satisfactory, albeit with lower discriminative ability (c-statistic: 0.71 & 0.61 at Hospitals A & B). Discriminative ability improved when model variables were individually refit on each cohort (c-statistics for Hospital A & B: 0.84 & 0.74). Decision-curve analyses showed benefit to use the calculators when average readmission risk was between 0-3%. Addition of SVI improved model fit (AIC 1850 vs 1533) for Hospital B, but not Hospital A (AIC 555 vs 523). C-statistics with SVI were 0.83 for Hospital A & 0.75 for Hospital B.
Conclusions Refitting a predictive model for postpartum HDP readmission demonstrated beneficial use in two cohorts in the southwestern US. The predictive model implemented in the hospital which serves a population with more adverse SDH did not demonstrate further improved discriminative ability by the addition of SVI. Postpartum readmission for HDP may be accurately predicted, likely after refitting this model to a health system’s cohort.
Hypothesis Model performance after external validation of a predictive model for PP HDP readmission would be enhanced by adding neighborhood-level SDH.
Methods Retrospective cohort study of deliveries from 2019-2022 using data from two hospital systems in Texas. PP readmission included inpatient stays with a diagnostic code of HDP occurring 1-42 days post-delivery discharge. Census-tract level Social Vulnerability Index (SVI) score was obtained using residential address at delivery. Site-specific model validation & recalibration were performed; models were assessed with concordance statistics (c- statistic) & Akaike information criterion (AIC), comparing the original calculator to the recalibrated & refit models, & the refit model with & without SVI.
Results Readmission frequency at Hospital A was 0.5% (48 readmissions/8,646 deliveries) & at Hospital B was 0.7% (163 readmissions/22,966 deliveries). Median SVI score was 0.84 & 0.46 in Hospitals A & B. Model performance using the original calculator (c-statistic 0.80) was satisfactory, albeit with lower discriminative ability (c-statistic: 0.71 & 0.61 at Hospitals A & B). Discriminative ability improved when model variables were individually refit on each cohort (c-statistics for Hospital A & B: 0.84 & 0.74). Decision-curve analyses showed benefit to use the calculators when average readmission risk was between 0-3%. Addition of SVI improved model fit (AIC 1850 vs 1533) for Hospital B, but not Hospital A (AIC 555 vs 523). C-statistics with SVI were 0.83 for Hospital A & 0.75 for Hospital B.
Conclusions Refitting a predictive model for postpartum HDP readmission demonstrated beneficial use in two cohorts in the southwestern US. The predictive model implemented in the hospital which serves a population with more adverse SDH did not demonstrate further improved discriminative ability by the addition of SVI. Postpartum readmission for HDP may be accurately predicted, likely after refitting this model to a health system’s cohort.
More abstracts on this topic:
Assessing Sex Differences in the Relationship Between Social Isolation and Incident Atherosclerotic Cardiovascular Disease and Death Using Data from the U.S. Health and Retirement Study
Graves Claire, Eisenberg-guyot Jerzy, Varghese Ashwini, Dodson John
Acceptability and Gain of Knowledge of Community Educational Tools About Rheumatic Heart Disease Integrated With Screening In Low-Income SettingsAbrams Jessica, Nunes Maria, Diniz Marina, Fraga Lucas, Paula Luiza, Coelho Cecilia, Tacuri Chavez Luz Marina, Lemos Larissa, Correia Julliane, Ribeiro Antonio, Nascimento Bruno, Sable Craig, Spaziani Alison, Zuhlke Liesl, Cardoso Clareci, Vinhal Wanessa, Ribeiro Isabely, Oliveira Kaciane, Amaral Ingred Beatriz