Final ID: MP602
Accessibility of Vascular Surgeons in Communities at High Risk for Peripheral Artery Disease
Abstract Body (Do not enter title and authors here): Background: Peripheral artery disease (PAD) is highly prevalent, but many patients face access challenges related to the number and distribution of vascular specialists. We hypothesized that integration of chronic disease prevalence and health behaviors with the population at risk would enhance identification of access-challenged communities versus established approaches based on total population and workforce counts.
Objective: Identify and characterize high-risk population access to vascular surgeons in the United States based on workforce distribution combined with community-level chronic disease, health risk, and population data.
Methods: Vascular surgeon locations were identified from the Physician Compare file from the Centers for Medicare and Medicaid Services. Surgeon accessibility was determined using an enhanced two-step floating catchment area, which accounts for the surgeon-to-demand ratio within each catchment area for adults over 50 years old. Population PAD risk was calculated utilizing a principal component analysis of crude prevalence rates of diabetes, hypertension, hyperlipidemia, obesity, and smoking at the zip-code level. Community-level access and characteristics were compared based on quartiles.
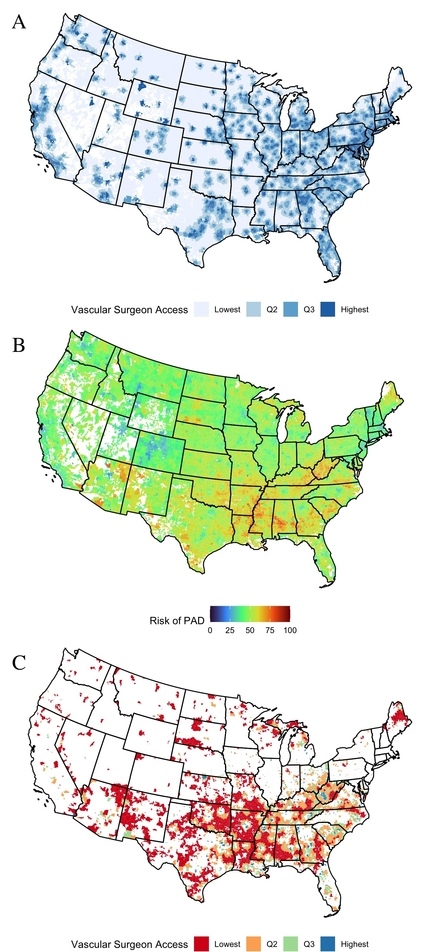
Results: The Mid-Atlantic region had the largest proportion (43.9%) of zip codes with access to vascular surgeons (Figure 1A), whereas the East South-Central region had the greatest proportion (68.7%) of zip codes with high PAD risk (Figure 1B). Among 8,077 high-risk PAD zip codes, 37.4% (n = 3,025) were categorized as having limited access to vascular surgeons. Limited access populations accounted for 20.7% (n=8,134,542) of the high-risk population. Over half (53%, n=4,288) of low-risk zip codes had high access to specialized care in comparison to only 9.9% (n=800) of high-risk communities (Figure 1C). High-risk PAD communities with low access to vascular surgeons were typically rural and isolated (40% vs. 0.9%, p<0.001), predominantly Non-Hispanic White (83% vs. 37%, p<0.001), and had lower median uninsured rates (11.5% vs. 13%, p<0.001) and poverty rates (17% vs. 26%, p<0.001) in contrast to other high-risk communities with greater access.
Conclusions: A substantial portion of high-risk PAD communities lack access to specialized vascular care. Use of population-level chronic disease and health risk behavior information can support targeted, community-level interventions to improve the mismatch between patient needs and workforce distribution.
Objective: Identify and characterize high-risk population access to vascular surgeons in the United States based on workforce distribution combined with community-level chronic disease, health risk, and population data.
Methods: Vascular surgeon locations were identified from the Physician Compare file from the Centers for Medicare and Medicaid Services. Surgeon accessibility was determined using an enhanced two-step floating catchment area, which accounts for the surgeon-to-demand ratio within each catchment area for adults over 50 years old. Population PAD risk was calculated utilizing a principal component analysis of crude prevalence rates of diabetes, hypertension, hyperlipidemia, obesity, and smoking at the zip-code level. Community-level access and characteristics were compared based on quartiles.
Results: The Mid-Atlantic region had the largest proportion (43.9%) of zip codes with access to vascular surgeons (Figure 1A), whereas the East South-Central region had the greatest proportion (68.7%) of zip codes with high PAD risk (Figure 1B). Among 8,077 high-risk PAD zip codes, 37.4% (n = 3,025) were categorized as having limited access to vascular surgeons. Limited access populations accounted for 20.7% (n=8,134,542) of the high-risk population. Over half (53%, n=4,288) of low-risk zip codes had high access to specialized care in comparison to only 9.9% (n=800) of high-risk communities (Figure 1C). High-risk PAD communities with low access to vascular surgeons were typically rural and isolated (40% vs. 0.9%, p<0.001), predominantly Non-Hispanic White (83% vs. 37%, p<0.001), and had lower median uninsured rates (11.5% vs. 13%, p<0.001) and poverty rates (17% vs. 26%, p<0.001) in contrast to other high-risk communities with greater access.
Conclusions: A substantial portion of high-risk PAD communities lack access to specialized vascular care. Use of population-level chronic disease and health risk behavior information can support targeted, community-level interventions to improve the mismatch between patient needs and workforce distribution.
More abstracts on this topic:
Biodegradable PLGA Nanoparticles Modulate Monocyte/Macrophage Actions Reduce Vein Wall Fibrosis
Moreno Oscar, Podojil Joseph, Cai Qing, Wakefield Thomas, Myers Daniel, Jaffer Farouc, Obi Andrea, Henke Peter, Parchment Nathaniel, Pellerito Mattea, Luke Catherine, Taylor Alessia, Micallef Kate, Taube Cole, Mccarthy Derrick, Elhofy Adam
A Comparative Analysis of Social Demographic and Clinical Factors for Screening for Peripheral Artery Disease in Adult Patients from Primary Care ClinicsLane Rashon, Jackson Pasha, Anokwuru Ferdinand, Dillard Naomi, Nerlekar Ridhima