Final ID: MP2276
Social Factors Associated with Pre-Pregnancy Care Utilization
Abstract Body (Do not enter title and authors here): Background: The American Heart Association recognizes the pre-pregnancy period as a window to optimize cardiovascular health and mitigate the risk of adverse pregnancy outcomes, particularly in those with cardiovascular disease (CVD) risk factors (RF). However, disparities in access to and utilization of preventive care are well-established outside of pregnancy. Understanding the social factors associated with lower pre-pregnancy care can inform interventions to improve equity in maternal health.
Methods: We used data from the Pregnancy Risk Assessment Monitoring System, a nationally representative survey of women with a recent live birth. We included women age ≥18 years with self-reported data on pre-pregnancy CVD RF (obesity, diabetes, hypertension, or tobacco use) and visit attendance. The primary outcome was attendance at a clinic visit (i.e., “regular checkup”) with an OB/GYN or primary care doctor in the year prior to pregnancy. We calculated age-adjusted odds of attendance in those with 0, 1 or > 2 of the following adverse social factors: poor transportation access, food insecurity, unstable housing, lack of health insurance, difficulty paying bills, history of domestic abuse, and lack of a high school education. Next, we conducted subgroup analyses by presence of 0, 1 or > 2 CVD RF. Analyses were weighted accounting for survey design.
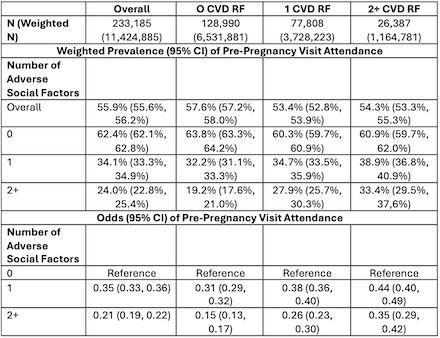
Results: Of 233,815 women (weighted N=11,424,885), the mean age was 29.5 years, 32.6% had 1 CVD RF, and 10.2% had >2 CVD RF. Adverse social factors were more often reported by those with CVD RF: 17.8% of those with no CVD RF, 25.7% with 1 CVD RF, and 28.3% with >2 CVD RF (p=<0.01). Overall frequency of a pre-pregnancy clinic visit was 55.9% with a lower frequency in those with higher burden of adverse social factors (TABLE). For example, odds of a pre-pregnancy clinic visit was lower in those with >2 compared with no adverse social factors in those with 0 CVD RF (63.8% VS 19.2%; aOR 0.15; 95% CI: 0.13-0.17), 1 CVD RF (60.3% VS 27.9%; aOR: 0.26; 95% CI: 0.23-0.30), and >2 CVD RF (60.9% VS 33.4%; aOR: 0.35; 95% CI: 0.29-0.42).
Conclusion: Adverse social factors are associated with a lower frequency of pre-pregnancy care utilization even among those with CVD RF. Among those with ≥2 adverse social factors, less than one-third of women attended a pre-pregnancy visit. Public health efforts should address upstream drivers of health to improve pre-pregnancy preventive care and optimize cardiovascular health.
Methods: We used data from the Pregnancy Risk Assessment Monitoring System, a nationally representative survey of women with a recent live birth. We included women age ≥18 years with self-reported data on pre-pregnancy CVD RF (obesity, diabetes, hypertension, or tobacco use) and visit attendance. The primary outcome was attendance at a clinic visit (i.e., “regular checkup”) with an OB/GYN or primary care doctor in the year prior to pregnancy. We calculated age-adjusted odds of attendance in those with 0, 1 or > 2 of the following adverse social factors: poor transportation access, food insecurity, unstable housing, lack of health insurance, difficulty paying bills, history of domestic abuse, and lack of a high school education. Next, we conducted subgroup analyses by presence of 0, 1 or > 2 CVD RF. Analyses were weighted accounting for survey design.
Results: Of 233,815 women (weighted N=11,424,885), the mean age was 29.5 years, 32.6% had 1 CVD RF, and 10.2% had >2 CVD RF. Adverse social factors were more often reported by those with CVD RF: 17.8% of those with no CVD RF, 25.7% with 1 CVD RF, and 28.3% with >2 CVD RF (p=<0.01). Overall frequency of a pre-pregnancy clinic visit was 55.9% with a lower frequency in those with higher burden of adverse social factors (TABLE). For example, odds of a pre-pregnancy clinic visit was lower in those with >2 compared with no adverse social factors in those with 0 CVD RF (63.8% VS 19.2%; aOR 0.15; 95% CI: 0.13-0.17), 1 CVD RF (60.3% VS 27.9%; aOR: 0.26; 95% CI: 0.23-0.30), and >2 CVD RF (60.9% VS 33.4%; aOR: 0.35; 95% CI: 0.29-0.42).
Conclusion: Adverse social factors are associated with a lower frequency of pre-pregnancy care utilization even among those with CVD RF. Among those with ≥2 adverse social factors, less than one-third of women attended a pre-pregnancy visit. Public health efforts should address upstream drivers of health to improve pre-pregnancy preventive care and optimize cardiovascular health.
More abstracts on this topic:
A Randomized Phase 2 Trial of Muvalaplin: An Oral Disrupter of the Assembly of Lipoprotein(a) Particles
Nicholls Stephen, Ni Wei, Rhodes Grace, Nissen Steven, Navar Ann Marie, Michael Laura, Krege John
A Multimodal Artificial Intelligence Signature of Advanced Cardiac and Vascular Aging Defines Elevated Risk of Cardiovascular DiseasePerera Sudheesha, Biswas Dhruva, Dhingra Lovedeep, Aminorroaya Arya, Coppi Andreas, Khera Rohan