Final ID: MP2535
Lytics or Leave it? Prosthetic Valve Thrombosis with Severe Aortic Insufficiency
Abstract Body (Do not enter title and authors here): Description of case: A 39-year-old man with history of unicuspid aortic valve status-post bicuspidization (2017), subsequent severe aortic insufficiency prompting mechanical aortic valve replacement (2023), recent prosthetic valve thrombosis on therapeutic warfarin complicated by stenosis and shock prompting redo mechanical aortic valve replacement (2/2025, 23mm On-X), presented with acute dyspnea, chest pain, and loss of mechanical click.
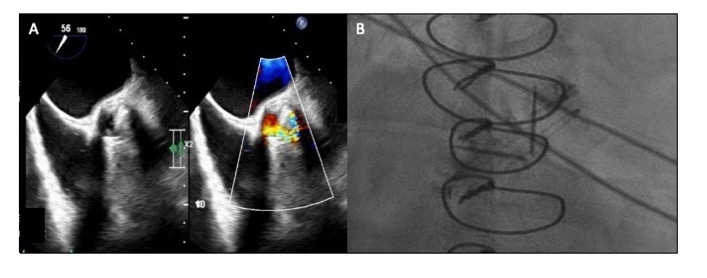
He was found to have SCAI-C cardiogenic shock, with exam notable for III/VI systolic crescendo-decrescendo and IV/IV decrescendo early diastolic murmurs, and absent mechanical click. Labs were notable for absolute eosinophils of 11.5 K/cu mm. On TTE, valve disks were poorly visualized. The mean gradient was 59mmHg and there was severe aortic insufficiency with preserved ventricular function. Due to concern for valvular obstruction, TEE was performed, revealing a well-seated valve with severe valvular regurgitation originating posteriorly and a reduction in systolic excursion of the disks. Valve fluoroscopy showed minimal movement of both discs suggesting thrombosis.
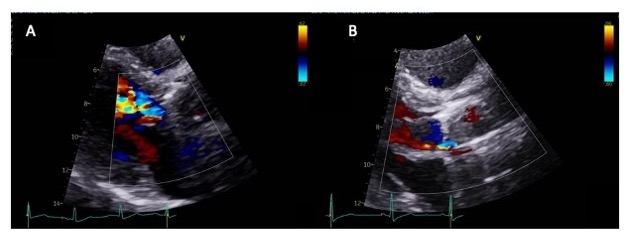
The patient was deemed high risk for surgical intervention and therefore received systemic thrombolysis with alteplase 25mg over 6h x2. Repeat TTE showed mean gradient 29mmHg, and mild-moderate aortic insufficiency. Eosinophilia peaked at 16.7 K/cu mm and normalized with high-dose prednisone. Eosinophilia workup is ongoing.
Discussion: Prosthetic valve thrombosis is a rare and feared complication without randomized controlled trials to support optimal treatment. The 2017 American Heart Association guidelines suggest surgery or fibrinolytics determined by individualized patient factors. Previously, surgery was preferred in patients with advanced NYHA symptoms or large thrombi. However, a novel strategy with echocardiogram-guided, low-dose infused fibrinolytics has demonstrated high success rates in this patient population. In our case, multimodal imaging was essential in the rapid diagnosis of prosthetic valve thrombosis. Our preference for fibrinolytics was based on surgical risk and to enable pre-operative workup and management of his hypercoagulable state. Few cases have been reported of eosinophilia-driven prosthetic valve thrombosis, with differential including eosinophilic granulomatosis polyangiitis and IgG4-related disease. Further data are needed to enable tailored treatment strategies in different patient populations.
He was found to have SCAI-C cardiogenic shock, with exam notable for III/VI systolic crescendo-decrescendo and IV/IV decrescendo early diastolic murmurs, and absent mechanical click. Labs were notable for absolute eosinophils of 11.5 K/cu mm. On TTE, valve disks were poorly visualized. The mean gradient was 59mmHg and there was severe aortic insufficiency with preserved ventricular function. Due to concern for valvular obstruction, TEE was performed, revealing a well-seated valve with severe valvular regurgitation originating posteriorly and a reduction in systolic excursion of the disks. Valve fluoroscopy showed minimal movement of both discs suggesting thrombosis.
The patient was deemed high risk for surgical intervention and therefore received systemic thrombolysis with alteplase 25mg over 6h x2. Repeat TTE showed mean gradient 29mmHg, and mild-moderate aortic insufficiency. Eosinophilia peaked at 16.7 K/cu mm and normalized with high-dose prednisone. Eosinophilia workup is ongoing.
Discussion: Prosthetic valve thrombosis is a rare and feared complication without randomized controlled trials to support optimal treatment. The 2017 American Heart Association guidelines suggest surgery or fibrinolytics determined by individualized patient factors. Previously, surgery was preferred in patients with advanced NYHA symptoms or large thrombi. However, a novel strategy with echocardiogram-guided, low-dose infused fibrinolytics has demonstrated high success rates in this patient population. In our case, multimodal imaging was essential in the rapid diagnosis of prosthetic valve thrombosis. Our preference for fibrinolytics was based on surgical risk and to enable pre-operative workup and management of his hypercoagulable state. Few cases have been reported of eosinophilia-driven prosthetic valve thrombosis, with differential including eosinophilic granulomatosis polyangiitis and IgG4-related disease. Further data are needed to enable tailored treatment strategies in different patient populations.
More abstracts on this topic:
Aortic Valve Calcification Density Performs Better Compared to Absolute Aortic Valve Calcification in Aortic Stenosis Risk Stratification
Ahmad Syed, Zeb Irfan, Watson Hangyu, Awad Maan, Patel Kunal, Nassar Sameh, Thyagaturu Harshith, Balla Sudarshan, Kawsara Mohammad, Daggubati Ramesh
A Novel Echocardiography Risk Score Predicted Mortality In Patients With Heart Failure With Preserved Ejection Fraction.Iwakura Katsuomi, Yoshio Yasumura, Hikoso Shungo, Okada Katsuki, Nakatani Daisaku, Sotomi Yohei, Sakata Yasushi, Tanaka Nobuaki, Okada Masato, Okamura Atsunori, Heitaro Watanabe, Seo Masahiro, Hayashi Takaharu, Yano Masamichi, Yamada Takahisa