Final ID: MP2288
Redefining Risk: Enhancing Prognostic Assessment in Primary Prevention with Coronary Artery Calcium Score
Abstract Body (Do not enter title and authors here): Introduction
Current CV prevention strategies focus on treating individuals based on estimated risk or clinical thresholds, but risk heterogeneity exists even within treatment-eligible groups. Coronary artery calcium (CAC) scoring may enhance risk assessment, but its added value across the entire risk spectrum remains uncertain. Using data from a multiethnic population-based cohort, we examined the association of CAC burden with major adverse cardiovascular events (MACE).
Methods
Adults aged 45–64 years without baseline ASCVD from the Multi-Ethnic Study of Atherosclerosis (MESA) were included. Participants were categorized into three mutually exclusive risk groups based on baseline pooled cohort equation (PCE) scores, LDL, systolic blood pressure (SBP), and diabetes status: therapy eligible intermediate-risk primary prevention, therapy eligible high-risk primary prevention, and therapy ineligible primordial prevention. CAC was categorized as 0, 1-<100, and ≥100 Agatston units. Cox proportional hazards models were used to assess the association between CAC categories and incident MACE across risk groups, adjusting for age, sex, race, body mass index (BMI), HDL cholesterol, triglycerides, and estimated glomerular filtration rate (eGFR). MACE was defined as a composite of hard CVD events, coronary revascularization, and cardiovascular death.
Results
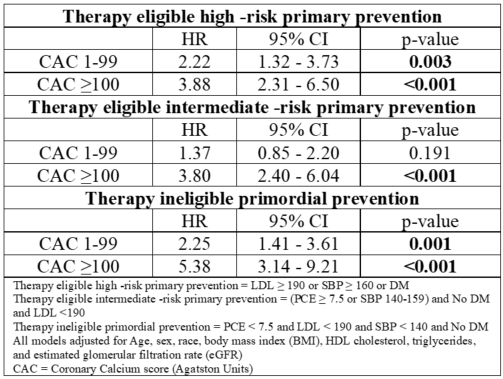
The cohort included 3,578 adults (mean age 54.6 years; 52.9% female; 27.6% African American), with a mean follow-up of 12.8 years. In fully adjusted models, higher CAC was independently associated with increased MACE risk across all risk groups. In the therapy eligible high-risk group, compared to CAC=0, the hazard ratio (HR) for CAC 1-99 was 2.22 (95% CI: 1.32-3.73; p=0.003) and 3.88 (95% CI: 2.31-6.50; p<0.001) for CAC ≥100. In the therapy eligible primary prevention group, HRs were 1.37 (95% CI: 0.85-2.19; p=0.191) for CAC 1-99 and 3.80 (95% CI: 2.40-6.04; p<0.0001) for CAC ≥100 (Table 1). In the therapy ineligible primordial prevention group, HRs were 2.25 (95% CI: 1.41-3.61; p=0.001) for CAC 1–99 and 5.38 (95% CI: 3.14-9.21; p<0.0001) for CAC ≥100.
Conclusion
Among treatment-eligible and ineligible adults, CAC provided independent and incremental prognostic information for MACE risk across the risk spectrum. These findings support the potential role of CAC testing to further individualize preventive strategies beyond traditional risk scores in both lower and higher risk populations.
Current CV prevention strategies focus on treating individuals based on estimated risk or clinical thresholds, but risk heterogeneity exists even within treatment-eligible groups. Coronary artery calcium (CAC) scoring may enhance risk assessment, but its added value across the entire risk spectrum remains uncertain. Using data from a multiethnic population-based cohort, we examined the association of CAC burden with major adverse cardiovascular events (MACE).
Methods
Adults aged 45–64 years without baseline ASCVD from the Multi-Ethnic Study of Atherosclerosis (MESA) were included. Participants were categorized into three mutually exclusive risk groups based on baseline pooled cohort equation (PCE) scores, LDL, systolic blood pressure (SBP), and diabetes status: therapy eligible intermediate-risk primary prevention, therapy eligible high-risk primary prevention, and therapy ineligible primordial prevention. CAC was categorized as 0, 1-<100, and ≥100 Agatston units. Cox proportional hazards models were used to assess the association between CAC categories and incident MACE across risk groups, adjusting for age, sex, race, body mass index (BMI), HDL cholesterol, triglycerides, and estimated glomerular filtration rate (eGFR). MACE was defined as a composite of hard CVD events, coronary revascularization, and cardiovascular death.
Results
The cohort included 3,578 adults (mean age 54.6 years; 52.9% female; 27.6% African American), with a mean follow-up of 12.8 years. In fully adjusted models, higher CAC was independently associated with increased MACE risk across all risk groups. In the therapy eligible high-risk group, compared to CAC=0, the hazard ratio (HR) for CAC 1-99 was 2.22 (95% CI: 1.32-3.73; p=0.003) and 3.88 (95% CI: 2.31-6.50; p<0.001) for CAC ≥100. In the therapy eligible primary prevention group, HRs were 1.37 (95% CI: 0.85-2.19; p=0.191) for CAC 1-99 and 3.80 (95% CI: 2.40-6.04; p<0.0001) for CAC ≥100 (Table 1). In the therapy ineligible primordial prevention group, HRs were 2.25 (95% CI: 1.41-3.61; p=0.001) for CAC 1–99 and 5.38 (95% CI: 3.14-9.21; p<0.0001) for CAC ≥100.
Conclusion
Among treatment-eligible and ineligible adults, CAC provided independent and incremental prognostic information for MACE risk across the risk spectrum. These findings support the potential role of CAC testing to further individualize preventive strategies beyond traditional risk scores in both lower and higher risk populations.
More abstracts on this topic:
A Loss of Function Polymorphism in the Propeptide of Lysyl Oxidase Exacerbates Atherosclerosis
Jung In-hyuk, Amrute Junedh, Luna Sophia, Wagoner Ryan, Lee Paul, Burks Kendall, Holloway Karyn, Alisio Arturo, Stitziel Nathan
A Qualitative Study of Perspectives on South Asian Dietary Practices: Exploring a Framework for Culturally Tailored Food-is-Medicine InterventionsKaloth Srivarsha, Fitzgerald Nurgul, Bacalia Karen Mae, Kalbag Aparna, Setoguchi Soko