Final ID: MP2271
A Health Coach-Based Multi-Level Personalized Strategy Lowers LDL-Cholesterol and Enhances Lipid Control in Veterans with Atherosclerotic Cardiovascular Disease – The VA Lipid Optimization Reimagined Quality Improvement Project at VA New York Harbor Healthcare System
Abstract Body (Do not enter title and authors here): Introduction: The VA New York Harbor Healthcare System (NYHHS) is one of 50 VA sites participating in a national quality improvement initiative called the VA Lipid Optimization Reimagined Quality Improvement Project (VALOR-QI). VALOR-QI is a collaborative project between the U.S. Department of Veterans Affairs (VA) and the American Heart Association (AHA) with the goal of positively impacting Veterans’ cardiovascular (CV) health. As part of the program, VA sites work with an AHA QI Consultant to develop and deploy a local QI plan to help overcome site specific barriers preventing Veterans from achieving optimal cholesterol levels (LDL-C).
Aims: To develop, implement, and evaluate a personalized approach for Veterans with ASCVD to achieve LDL-C control (<70 mg/dL).
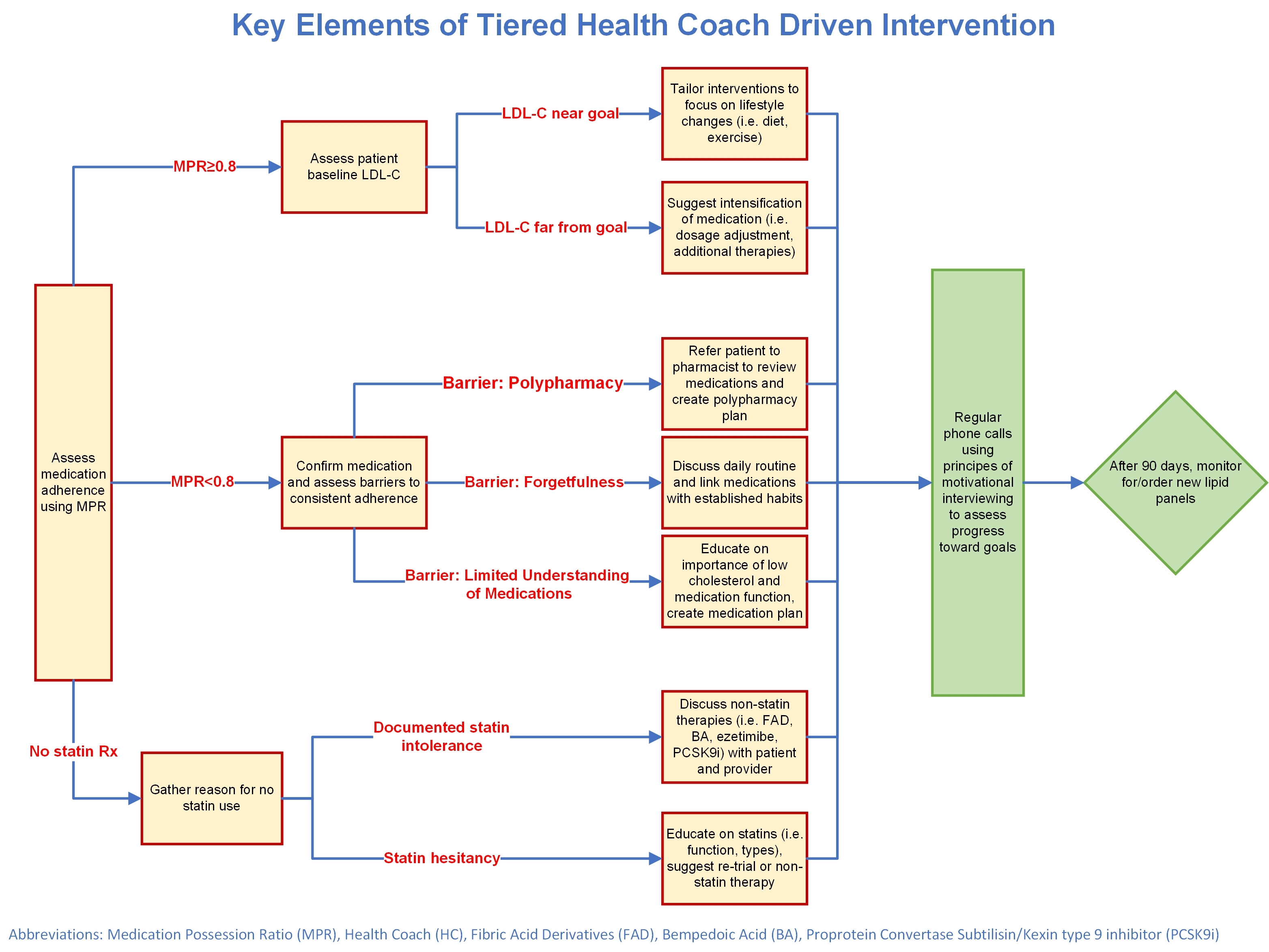
Methods: Health Coaches (HCs) used feedback from primary care, cardiology, geriatrics, endocrinology, and neurology providers; the literature; and local system knowledge to refine and develop enrollment plans and tiered intervention strategies (Fig 1). HCs used motivational interviewing (MI) to coach on medication routines, lifestyle habits, and LDL-C literacy. Using medication possession ratio (MPR) to assess adherence, HCs tailored coaching with MI and made pharmacy referrals (if MPR<0.8) or suggested medication intensification (if MPR≥0.8). We compared baseline and follow-up data to evaluate LDL-C lowering (Wilcoxon Signed-Rank and Kruskal-Wallis tests) and LDL-C control (Binomial tests and Fisher’s Exact tests).
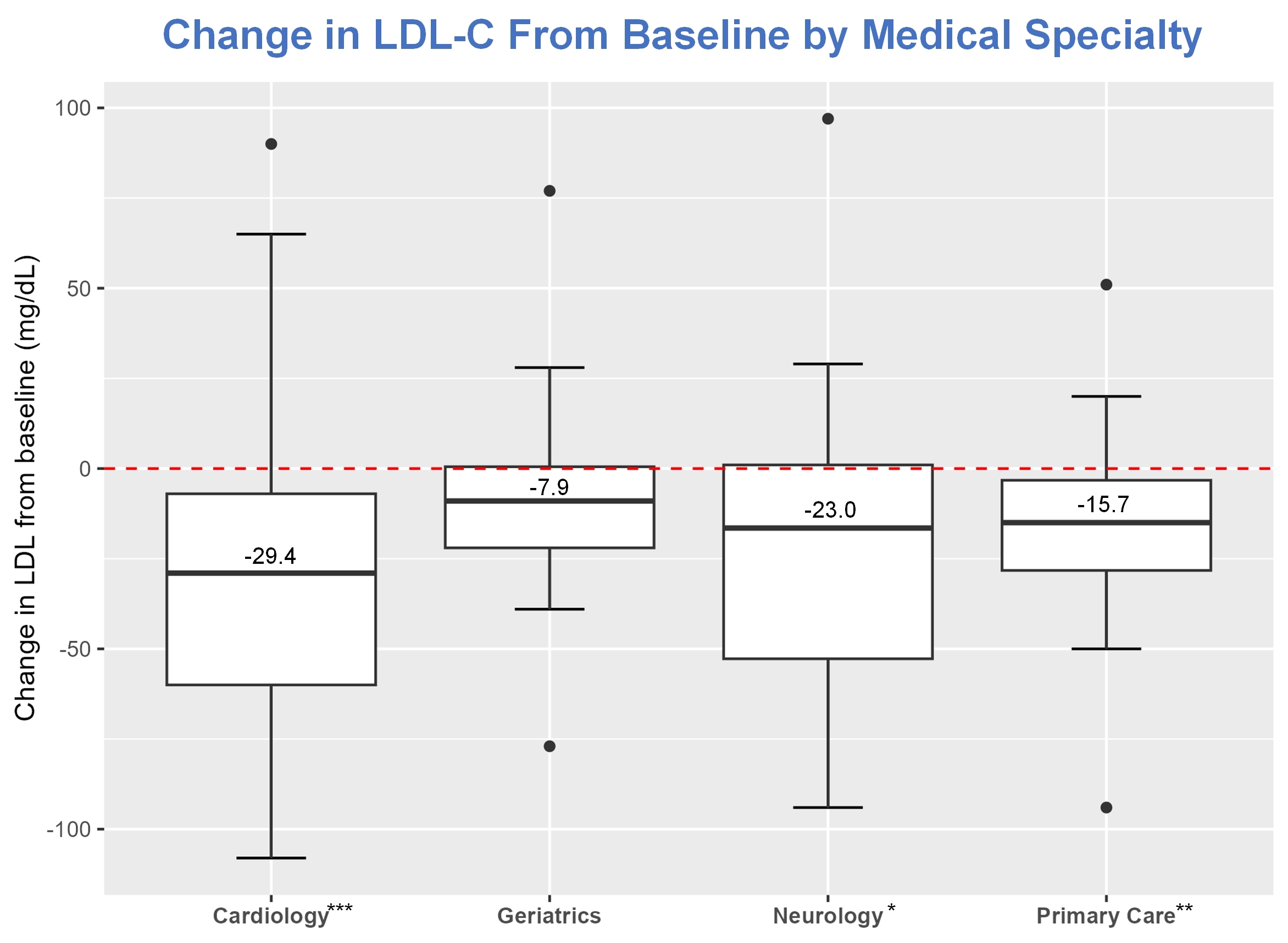
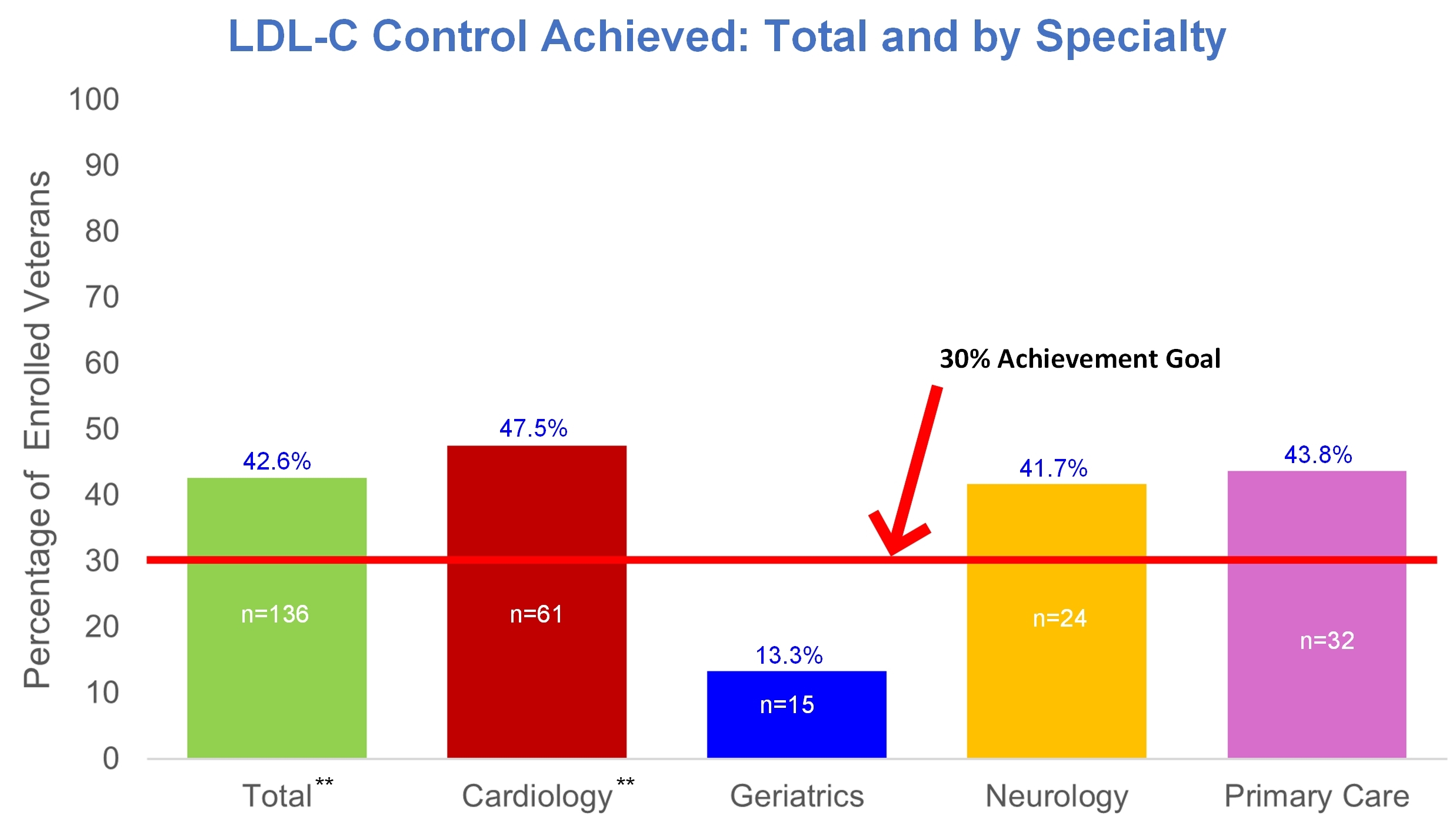
Results: We enrolled 152 Veterans. Median age was 74 years, 144 (94.7%) were male, 64 (42.1%) had DM, 141 (92.8%) had HTN, and 48 (31.6%) had BMI>30. At baseline, 88 (57.9%) had 70 mg/dL≤LDL-C<100 mg/dL, 63 (41.4%) had LDL-C≥100 mg/dL, and 1 (0.7%) had no data in the last year. Median baseline LDL-C was 92.0 mg/dL; follow-up 76.0 mg/dL. Mean change in LDL-C from baseline was -22.7 mg/dL (Wilcoxon Signed Rank test p<0.001). The proportion with LDL-C<70 mg/dL was 42.6%, higher than the benchmark goal of 30% (Binomial test p=0.001). All specialties, except geriatrics, had significant LDL-C lowering (Fig 2) and exceeded the 30% goal (Fig 3). LDL-C control rates did not statistically differ by specialty (Fisher’s Exact test p=0.091).
Conclusions: HC interventions optimized lipids in Veterans with ASCVD. Medication adherence was the greatest challenge to lipid lowering on a patient-level. Lack of provider consensus on LDL-C target, especially in geriatrics, was the main system-level barrier.
Aims: To develop, implement, and evaluate a personalized approach for Veterans with ASCVD to achieve LDL-C control (<70 mg/dL).
Methods: Health Coaches (HCs) used feedback from primary care, cardiology, geriatrics, endocrinology, and neurology providers; the literature; and local system knowledge to refine and develop enrollment plans and tiered intervention strategies (Fig 1). HCs used motivational interviewing (MI) to coach on medication routines, lifestyle habits, and LDL-C literacy. Using medication possession ratio (MPR) to assess adherence, HCs tailored coaching with MI and made pharmacy referrals (if MPR<0.8) or suggested medication intensification (if MPR≥0.8). We compared baseline and follow-up data to evaluate LDL-C lowering (Wilcoxon Signed-Rank and Kruskal-Wallis tests) and LDL-C control (Binomial tests and Fisher’s Exact tests).
Results: We enrolled 152 Veterans. Median age was 74 years, 144 (94.7%) were male, 64 (42.1%) had DM, 141 (92.8%) had HTN, and 48 (31.6%) had BMI>30. At baseline, 88 (57.9%) had 70 mg/dL≤LDL-C<100 mg/dL, 63 (41.4%) had LDL-C≥100 mg/dL, and 1 (0.7%) had no data in the last year. Median baseline LDL-C was 92.0 mg/dL; follow-up 76.0 mg/dL. Mean change in LDL-C from baseline was -22.7 mg/dL (Wilcoxon Signed Rank test p<0.001). The proportion with LDL-C<70 mg/dL was 42.6%, higher than the benchmark goal of 30% (Binomial test p=0.001). All specialties, except geriatrics, had significant LDL-C lowering (Fig 2) and exceeded the 30% goal (Fig 3). LDL-C control rates did not statistically differ by specialty (Fisher’s Exact test p=0.091).
Conclusions: HC interventions optimized lipids in Veterans with ASCVD. Medication adherence was the greatest challenge to lipid lowering on a patient-level. Lack of provider consensus on LDL-C target, especially in geriatrics, was the main system-level barrier.
More abstracts on this topic:
A 3-Year, Pre-Trial, Real-world Data Analysis of Patients Enrolled in VICTORION-INITIATE: Insights Using Tokenization
Rodriguez Fatima, Cosmatos Irene, Desai Nihar, Wright R, Ross Elsie, Ali Yousuf, Kumar Biswajit, Han Guangyang, Cai Beilei, Abbas Cheryl, Ryan Amy
A Comprehensive Study on Machine Learning Models Combining with Oversampling for One-year Persistent Coronary Artery Aneurysm in Kawasaki DiseaseLiang Kaizhi, Pang Yusheng, Su Danyan