Final ID: MP288
Vasoactive medications in the management of normotensive cardiogenic shock: patient factors and provider choices affecting the likelihood of mortality
Abstract Body (Do not enter title and authors here): Introduction: Though there are well-described unmodifiable factors known to affect survival from cardiogenic shock (CS), key questions remain regarding vasoactive medication (VM) management in less common subtypes such as normotensive CS. Understanding the impact of VM choice is key to optimizing outcomes in this specific sub-type of CS.
Question: Does the selection and order of VMs (inotrope, nitroprusside) impact survival in normotensive CS?
Methods: Patients admitted to the cardiac intensive care unit (CICU) of an academic medical center with CS between 2015-2024 were identified based on ICD-10 code for “Cardiogenic Shock” and most recent LVEF <40%, lactate >2 mmol/L, and initial SBP >90 with manual chart review confirmation of CS requiring VM. The primary outcome was the proportion of patients who survived to hospital discharge and/or heart failure advanced therapy. Predictors included order of VM, time to VM administration following first abnormal lactate, demographics, and clinical characteristics. Random forest modeling was used to identify key contributors to sample variance. These variables were then included in bootstrapped models of the primary outcome.
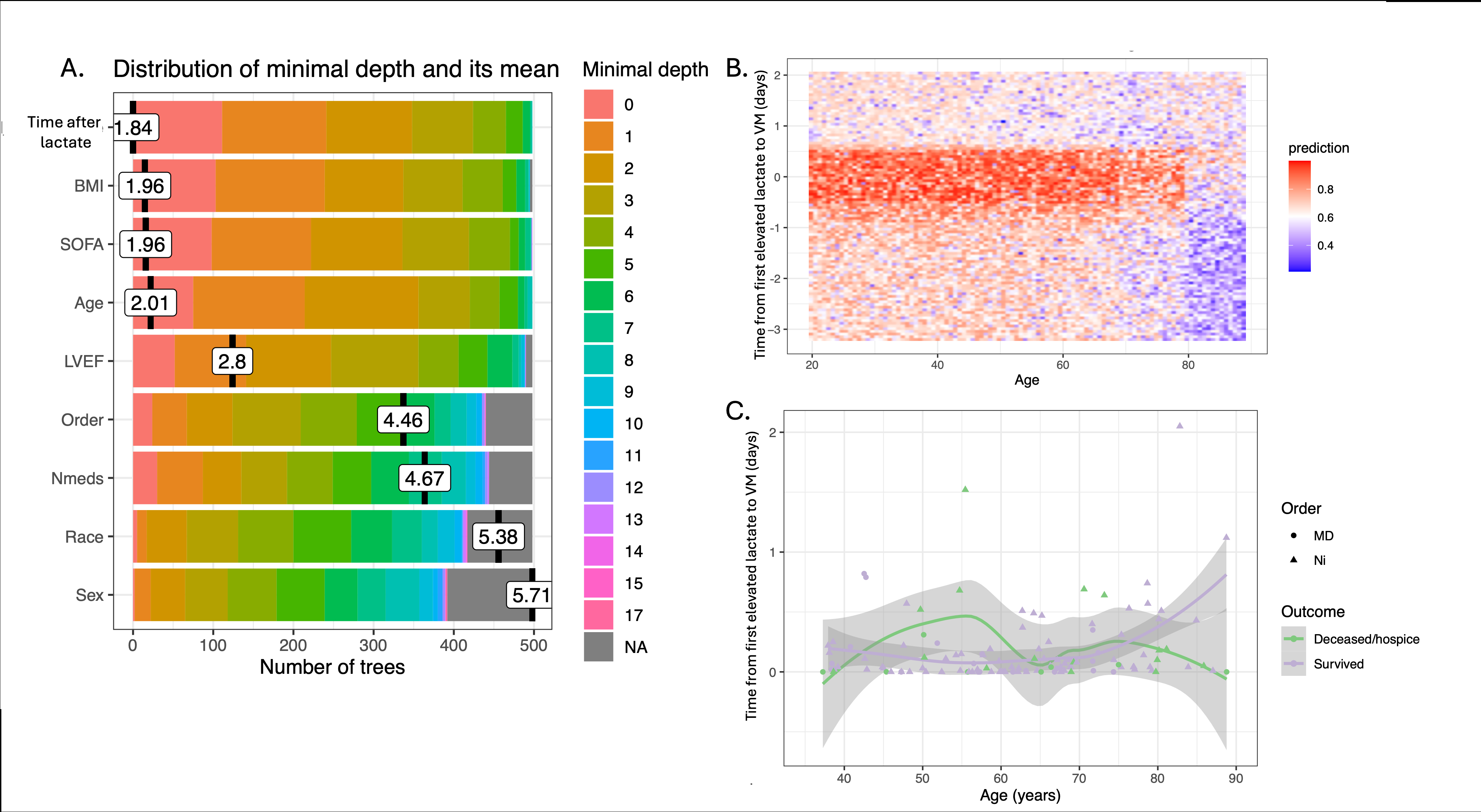
Results: 130 individuals were eligible for analysis, of whom 106 survived (81.5%). Those who survived were younger (58.4 v 64.3 years, p= 0.09) with a lower body mass index (25.9 kg/m2 v 29.0 kg/m2, p=0.07). The random forest model (Figure 1a) additionally identified LVEF, sequential organ failure assessment (SOFA) score, number of VMs, and order of VMs as survival differentiating. Number and order of VMs were noted to interact with patient age and SOFA score in predicting survival. Those who were older, received more VMs, and received milrinone or dobutamine prior to an elevated lactate had a lower likelihood of survival (ARR -0.27, p= 0.036, Figure 1b and 1c). Conversely, lower SOFA score, younger age, and having received nitroprusside first predicted survival in the bootstrapped logistic regression model (CI 3.4, 281.7).
Conclusion: In this single-center retrospective study of predictors of survival in normotensive CS, the interaction of being younger, having a lower SOFA score, and receiving nitroprusside as first VM conferred a higher chance of survival. VM choice should be further investigated in a larger, multisite cohort to inform VM treatment recommendations.
Question: Does the selection and order of VMs (inotrope, nitroprusside) impact survival in normotensive CS?
Methods: Patients admitted to the cardiac intensive care unit (CICU) of an academic medical center with CS between 2015-2024 were identified based on ICD-10 code for “Cardiogenic Shock” and most recent LVEF <40%, lactate >2 mmol/L, and initial SBP >90 with manual chart review confirmation of CS requiring VM. The primary outcome was the proportion of patients who survived to hospital discharge and/or heart failure advanced therapy. Predictors included order of VM, time to VM administration following first abnormal lactate, demographics, and clinical characteristics. Random forest modeling was used to identify key contributors to sample variance. These variables were then included in bootstrapped models of the primary outcome.
Results: 130 individuals were eligible for analysis, of whom 106 survived (81.5%). Those who survived were younger (58.4 v 64.3 years, p= 0.09) with a lower body mass index (25.9 kg/m2 v 29.0 kg/m2, p=0.07). The random forest model (Figure 1a) additionally identified LVEF, sequential organ failure assessment (SOFA) score, number of VMs, and order of VMs as survival differentiating. Number and order of VMs were noted to interact with patient age and SOFA score in predicting survival. Those who were older, received more VMs, and received milrinone or dobutamine prior to an elevated lactate had a lower likelihood of survival (ARR -0.27, p= 0.036, Figure 1b and 1c). Conversely, lower SOFA score, younger age, and having received nitroprusside first predicted survival in the bootstrapped logistic regression model (CI 3.4, 281.7).
Conclusion: In this single-center retrospective study of predictors of survival in normotensive CS, the interaction of being younger, having a lower SOFA score, and receiving nitroprusside as first VM conferred a higher chance of survival. VM choice should be further investigated in a larger, multisite cohort to inform VM treatment recommendations.
More abstracts on this topic:
Admission Cell-free DNA Predicts Cardiogenic Shock Progression and In-Hospital Mortality
Park Ashley, Kong Hyesik, Andargie Temesgen, Jang Moon, Solomon Michael, Brusca Samuel, Barnett Christopher, Obrien Connor, Agbor-enoh Sean
Acute and Chronic Phosphorylation of CaMKII on Coronary Microvascular/Endothelial FunctionIddrisu Hanisah, Xing Hang, Shi Guangbin, Liu Yuhong, Feng Jun