Final ID: Su902
Ability of Composite Magnetic Resonance Brain Imaging Scores to Predict Functional Outcomes in Survivors of Cardiac Arrest
Abstract Body: Background: Brain magnetic resonance imaging (MRI) has been examined for neuroprognostication (NP) after out-of-hospital cardiac arrest (OHCA). However, studies have focused on predicting poor outcomes of non-awakening and/or death. Recommendations for utilization of brain MRI in NP remain weak due to its subjective interpretation.
Aim: We modified a previously published brain MRI score and examined our quantitated NP scores’ ability to predict good functional outcomes in OHCA survivors.
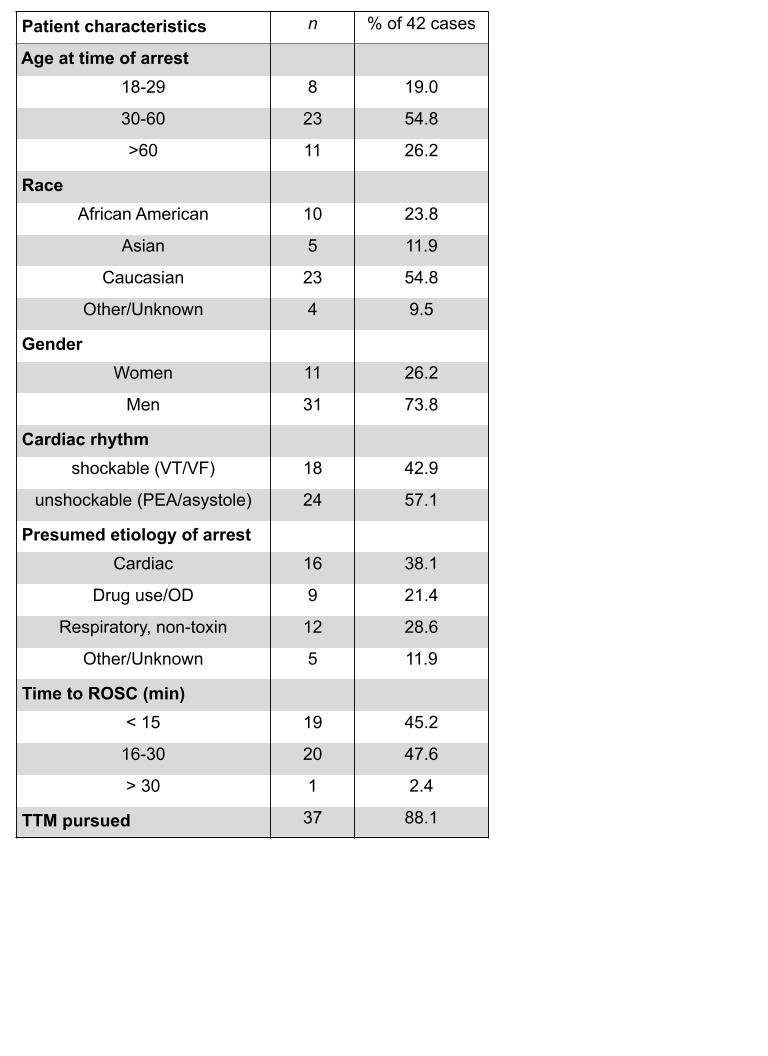
Methods: We screened OHCA cases (2017-2023, Seattle Medic One registry) for patients who survived to hospital discharge and had brain MRIs performed 25 hours-7 days after arrest. Each MRI was reviewed by two adjudicators; a third reviewer served as tie-breaker. Reviewers were blinded to patient outcomes. Diffusion Weighted Imaging and Fluid Attenuated Inversion Recovery sequences were reviewed to score 35 neuroanatomical regions. Graded severity for estimated affected area (0 = zero; 1= < 25%; 2 = 25-50%; 3 = 50-75%; 4 = >75%) and binary (0 = not affected, 1 = affected) scores were tallied. Points were summed for a composite brain MRI score, “NP score”, possible range 0-214. Primary outcome was Cerebral Performance Categories (CPC) at hospital discharge (1-2: “independent”, 3: “dependent”, 4: “vegetative state”). Computational modeling employed folded normal distributions and Maximum Likelihood Estimation. Statistical analyses were Pearson’s, Spearman’s, ANOVA, Fisher LSD, t-tests.
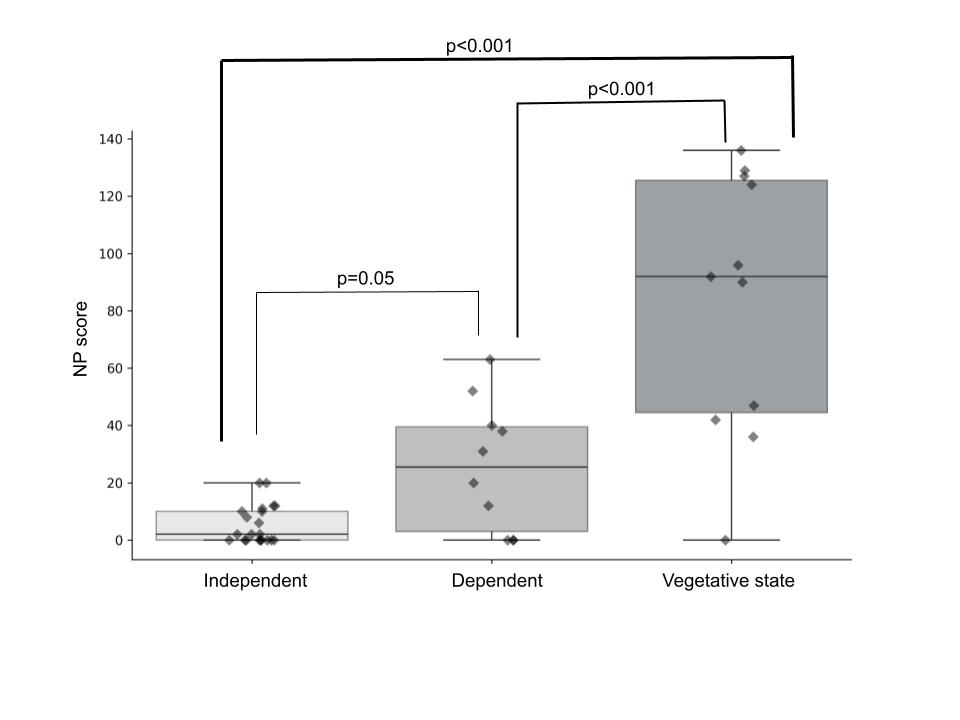
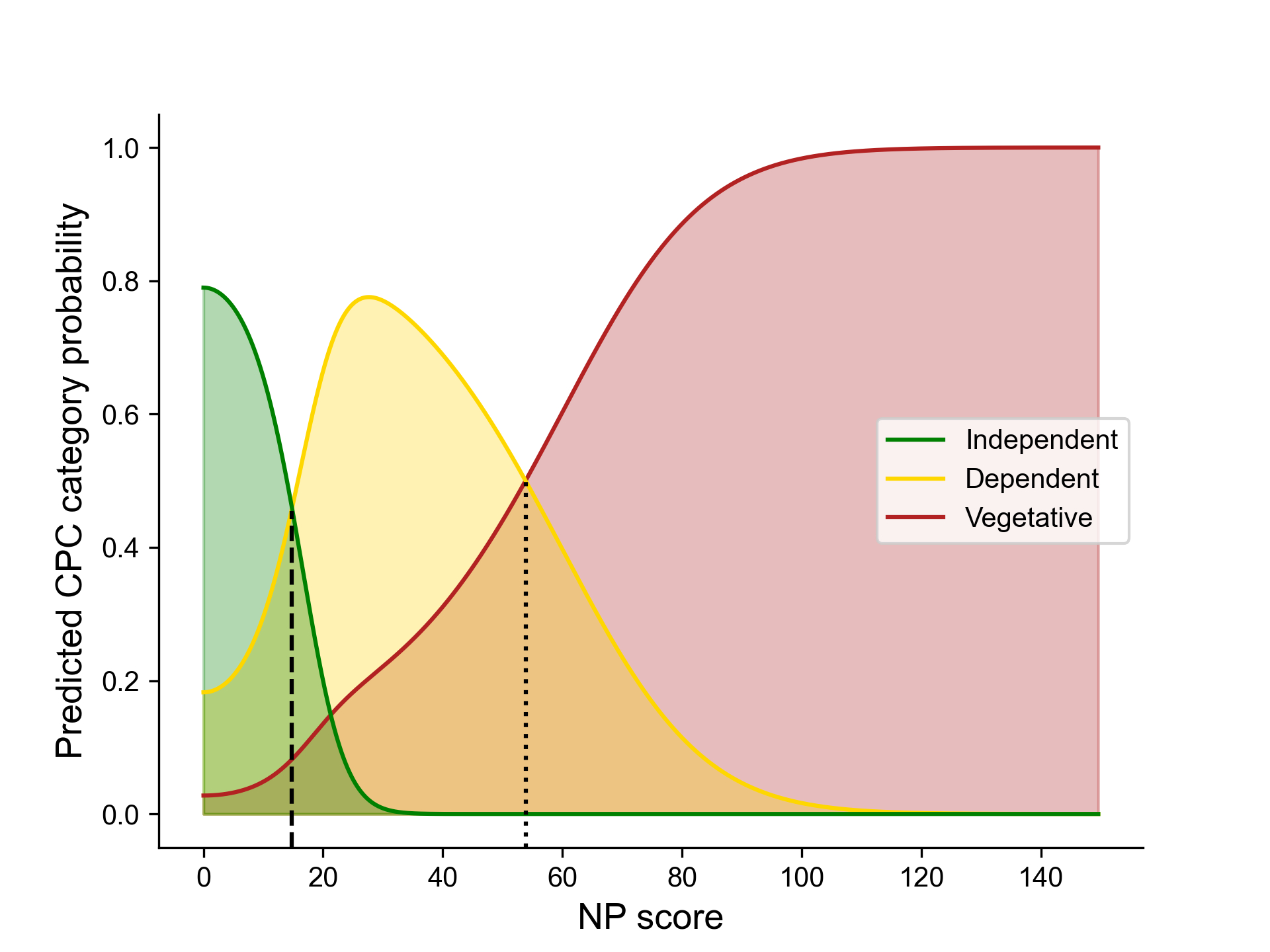
Results: Forty-two (42) adult patients were included (74% men, 55% Caucasian). Median NP score was 11.5 (IQR 41.5, n=42) overall, 2 (IQR=10, n=21) for independent versus 25.5 (IQR 36.5, n=10) for dependent patients, and 92 (IQR=81, n=11) for those in a vegetative state. NP scores strongly correlated with CPC [rs (40) = .69, p< .001], and were significantly different between CPC groups [F(2,39) = 32.66, p< 0.001]. Interrater concordance for NP score was high (Pearson) r = .88 [r = .96; .95; .90; .71].
Conclusions: Our NP score correlated well with good functional outcomes in OHCA survivors, and (1) identified distinct thresholds that well-separate functional outcome groups and (2) had very strong concordance rate among four pairs of adjudicators. NP score-based predictive modeling differentiates functional outcomes beyond good versus poor dichotomy and may help providers and family anticipate recovery potential.
Aim: We modified a previously published brain MRI score and examined our quantitated NP scores’ ability to predict good functional outcomes in OHCA survivors.
Methods: We screened OHCA cases (2017-2023, Seattle Medic One registry) for patients who survived to hospital discharge and had brain MRIs performed 25 hours-7 days after arrest. Each MRI was reviewed by two adjudicators; a third reviewer served as tie-breaker. Reviewers were blinded to patient outcomes. Diffusion Weighted Imaging and Fluid Attenuated Inversion Recovery sequences were reviewed to score 35 neuroanatomical regions. Graded severity for estimated affected area (0 = zero; 1= < 25%; 2 = 25-50%; 3 = 50-75%; 4 = >75%) and binary (0 = not affected, 1 = affected) scores were tallied. Points were summed for a composite brain MRI score, “NP score”, possible range 0-214. Primary outcome was Cerebral Performance Categories (CPC) at hospital discharge (1-2: “independent”, 3: “dependent”, 4: “vegetative state”). Computational modeling employed folded normal distributions and Maximum Likelihood Estimation. Statistical analyses were Pearson’s, Spearman’s, ANOVA, Fisher LSD, t-tests.
Results: Forty-two (42) adult patients were included (74% men, 55% Caucasian). Median NP score was 11.5 (IQR 41.5, n=42) overall, 2 (IQR=10, n=21) for independent versus 25.5 (IQR 36.5, n=10) for dependent patients, and 92 (IQR=81, n=11) for those in a vegetative state. NP scores strongly correlated with CPC [rs (40) = .69, p< .001], and were significantly different between CPC groups [F(2,39) = 32.66, p< 0.001]. Interrater concordance for NP score was high (Pearson) r = .88 [r = .96; .95; .90; .71].
Conclusions: Our NP score correlated well with good functional outcomes in OHCA survivors, and (1) identified distinct thresholds that well-separate functional outcome groups and (2) had very strong concordance rate among four pairs of adjudicators. NP score-based predictive modeling differentiates functional outcomes beyond good versus poor dichotomy and may help providers and family anticipate recovery potential.
More abstracts on this topic:
Comparison of Anti-coagulation and anti-Platelet Therapies for Intracranial Vascular Atherostenosis-Magnetic Resonance Imaging (CAPTIVA-MRI)
Wong Ka-ho, De Havenon Adam, Sulken Amy, Knebusch Clara, Reed Rachel, Faraco Carlos, Martin Renee, Amin-hanjani Sepideh, Chatterjee Arindam, Liebeskind David
An Unusual but Clinically Significant Mechanism of Cerebral Fat Embolism Syndrome in Sickle Cell Disease Patient via Patent Foramen OvaleObeng Samed, Odukudu God-dowell, Amadi Chima, Ford Dimitri, Azees Ridwan, Saint Julien Berlandson, Opare-addo Michael S. N.