Final ID: Mo3084
Genetic Counseling Trends Amongst Cardiomyopathy Associated with Pregnancy
Abstract Body (Do not enter title and authors here): Background: Cardiomyopathy (CM)- including peripartum (PPCM) and other subtypes of dilated cardiomyopathy (DCM)- significantly contribute to maternal morbidity and mortality. Genetic testing to identify pathologic variants is recommended for DCM, though guidelines for PPCM are not clear. Genetic testing around pregnancy has both maternal and fetal implications, yet referral to genetic counseling (GC) is uncommon. We sought to determine the frequency of GC referrals among patients with PPCM and DCM in a Cardio-Obstetrics Program and whether referrals were influenced by social determinants of health.
Methods: We conducted a single-center, retrospective cohort study of with an ICD-10 code for DCM or PPCM and a documented birth between 2012-2025. Natural language processing tools were used to search progress notes for “genetic counsel*”. Results were manually reviewed for attempted referrals to GC for maternal indications; attempts were used instead of referrals to account for patients declining referral. Patient insurance type (public vs private), census tract data based on ZIP code of residence (median family income, presence of a local hospital, education ratio) were used to create a four-point, social determinants index ranked by “least”, “moderate”, and “most” affluence/access by indicators. Logistic regression models and bootstrapped probability distributions were used to characterize the likelihood of attempted genetic counseling referral by CM type and affluence/access category.
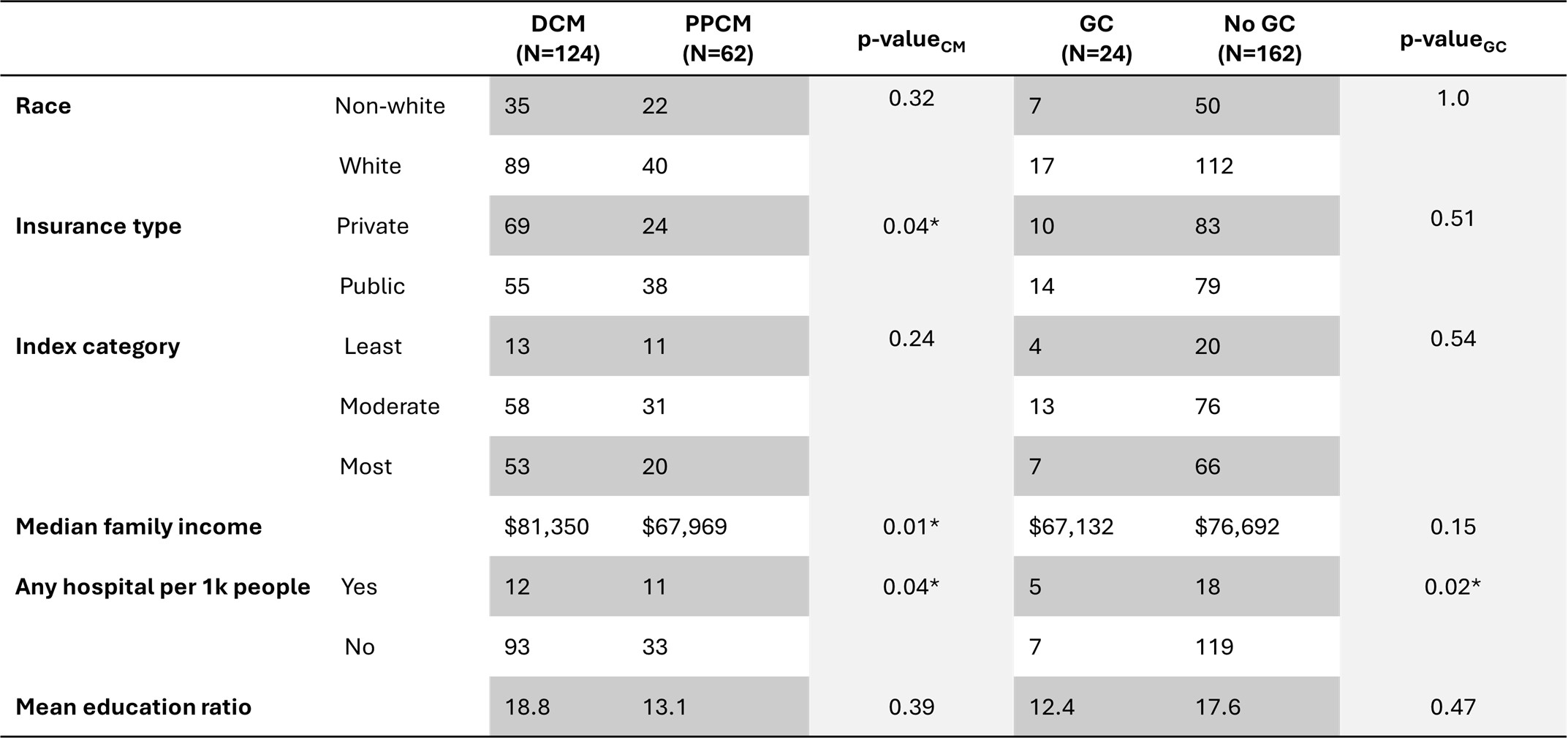
Results: 186 patients were eligible for analysis; 12.9% (24/186) had documented GC referral attempts. Those living in a census tract with a hospital were more likely to have an attempted referral (p=0.02, Table 1). Rates of genetic counseling did not differ based on race (p=1.0). There was no difference in documented GC referral attempts between patients diagnosed with DCM vs PPCM (10% vs 18%, p=0.17). Attempts were distributed similarly across affluence/access categories (10% in ‘most’ vs 15% in ‘moderate’ vs 17% in ‘least’, p=0.54, Figure 1). Notably, 2 individuals were diagnosed with pathogenic maternal variants via follow-up of fetal testing rather than maternal referral.
Conclusion: GC impacts both care of individuals with CM and their children. Pregnancy provides a unique window for access to healthcare. Despite this, whether patients have DCM or PPCM, rates of GC remain low irrespective of measures of socioeconomic status or race, which are historically barriers to care.
Methods: We conducted a single-center, retrospective cohort study of with an ICD-10 code for DCM or PPCM and a documented birth between 2012-2025. Natural language processing tools were used to search progress notes for “genetic counsel*”. Results were manually reviewed for attempted referrals to GC for maternal indications; attempts were used instead of referrals to account for patients declining referral. Patient insurance type (public vs private), census tract data based on ZIP code of residence (median family income, presence of a local hospital, education ratio) were used to create a four-point, social determinants index ranked by “least”, “moderate”, and “most” affluence/access by indicators. Logistic regression models and bootstrapped probability distributions were used to characterize the likelihood of attempted genetic counseling referral by CM type and affluence/access category.
Results: 186 patients were eligible for analysis; 12.9% (24/186) had documented GC referral attempts. Those living in a census tract with a hospital were more likely to have an attempted referral (p=0.02, Table 1). Rates of genetic counseling did not differ based on race (p=1.0). There was no difference in documented GC referral attempts between patients diagnosed with DCM vs PPCM (10% vs 18%, p=0.17). Attempts were distributed similarly across affluence/access categories (10% in ‘most’ vs 15% in ‘moderate’ vs 17% in ‘least’, p=0.54, Figure 1). Notably, 2 individuals were diagnosed with pathogenic maternal variants via follow-up of fetal testing rather than maternal referral.
Conclusion: GC impacts both care of individuals with CM and their children. Pregnancy provides a unique window for access to healthcare. Despite this, whether patients have DCM or PPCM, rates of GC remain low irrespective of measures of socioeconomic status or race, which are historically barriers to care.
More abstracts on this topic:
A Nationwide Italian Network for the Clinical and Genetic Diagnosis of Familial Dyslipidemias: The LIPIGEN registry
Casula Manuela, Galimberti Federica, Olmastroni Elena, Arca Marcello, Averna Maurizio, Catapano Alberico
Abnormal Calcium Regulation Leads to Pathological Cardiac Hypertrophy During Pregnancy in the GSNOR-Deficient Mouse Model of PreeclampsiaDulce Raul, Balkan Wayne, Hare Joshua, Kulandavelu Shathiyah