Final ID: MP40
Intersecting Inequities: Mapping Racial and Social Vulnerability Hotspots in U.S. Cardiogenic Shock Mortality
Abstract Body (Do not enter title and authors here): Background
Cardiogenic shock [CS] remains highly lethal. Whether county-level structural vulnerabilities, as captured by the CDC Social Vulnerability Index [SVI], modify racial mortality gaps is unknown.
Objective
To quantify area-specific CS mortality gradients across SVI quartiles and to map high-burden hotspots.
Methods
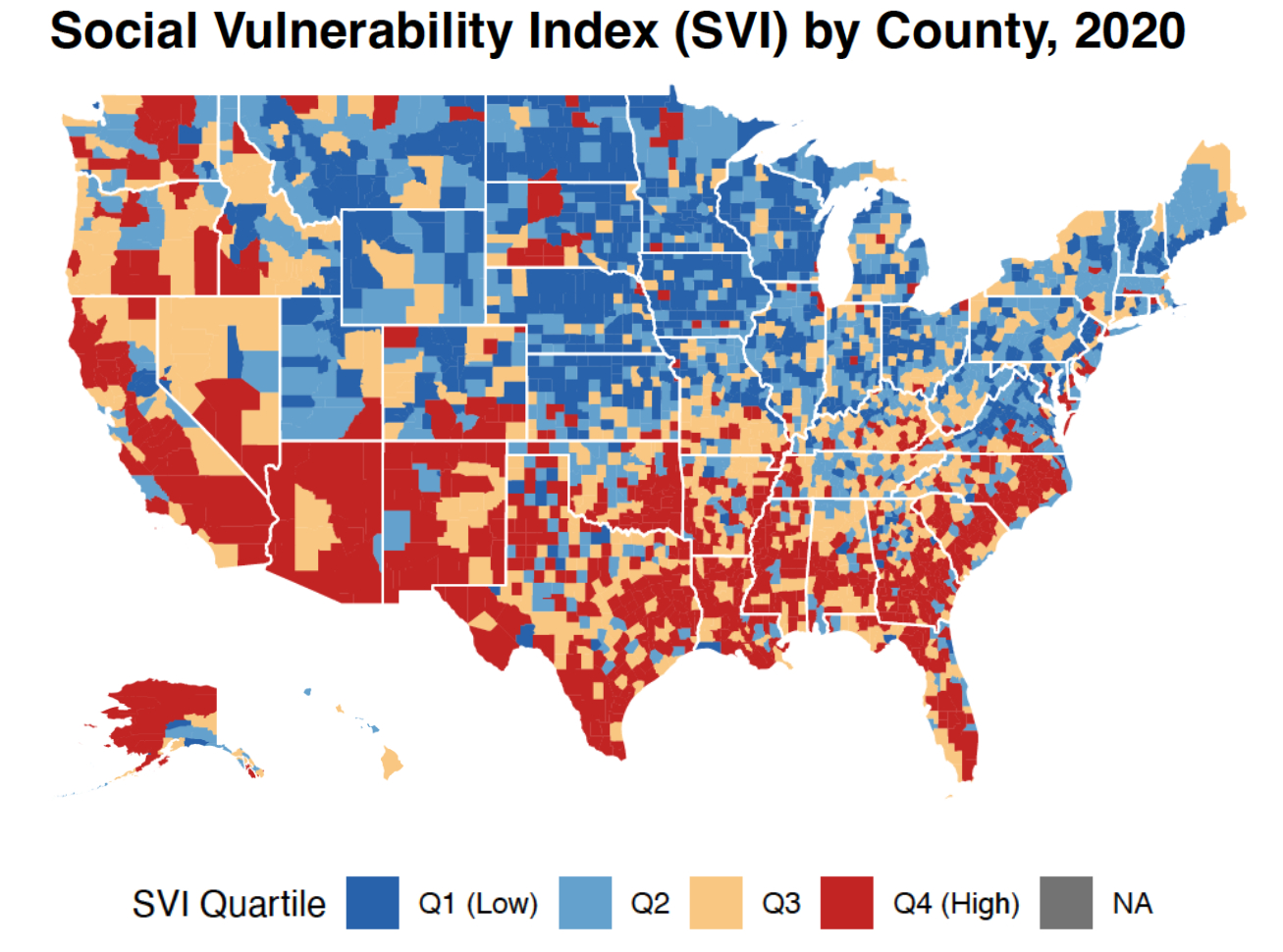
We extracted mortality data about CS from CDC WONDER [2016–2020] and merged it with 2020 CDC SVI data. Age-adjusted mortality rates [AAMRs, per 100,000] were calculated for American Indian/Alaska Native [AIAN], Asian/Pacific Islander [API], Black, Hispanic, and White populations stratified by SVI quartile [Q1 being least, Q4 being most vulnerable]. One-way ANOVA tested AAMR differences across quartiles [alpha equal to 0.05]. Counties in Q4 whose race-specific AAMR exceeded the 95th percentile were designated hotspots.
Results
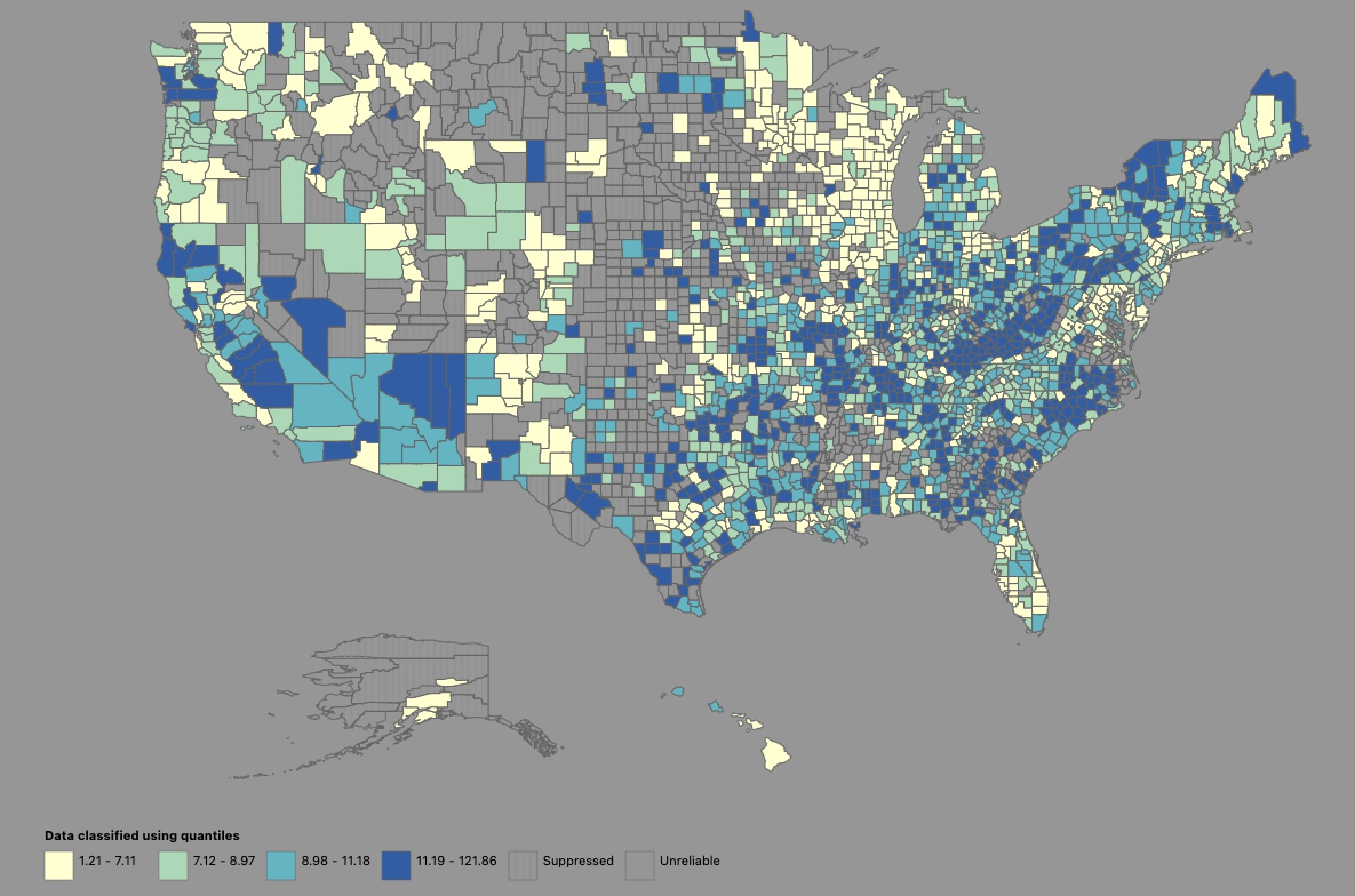
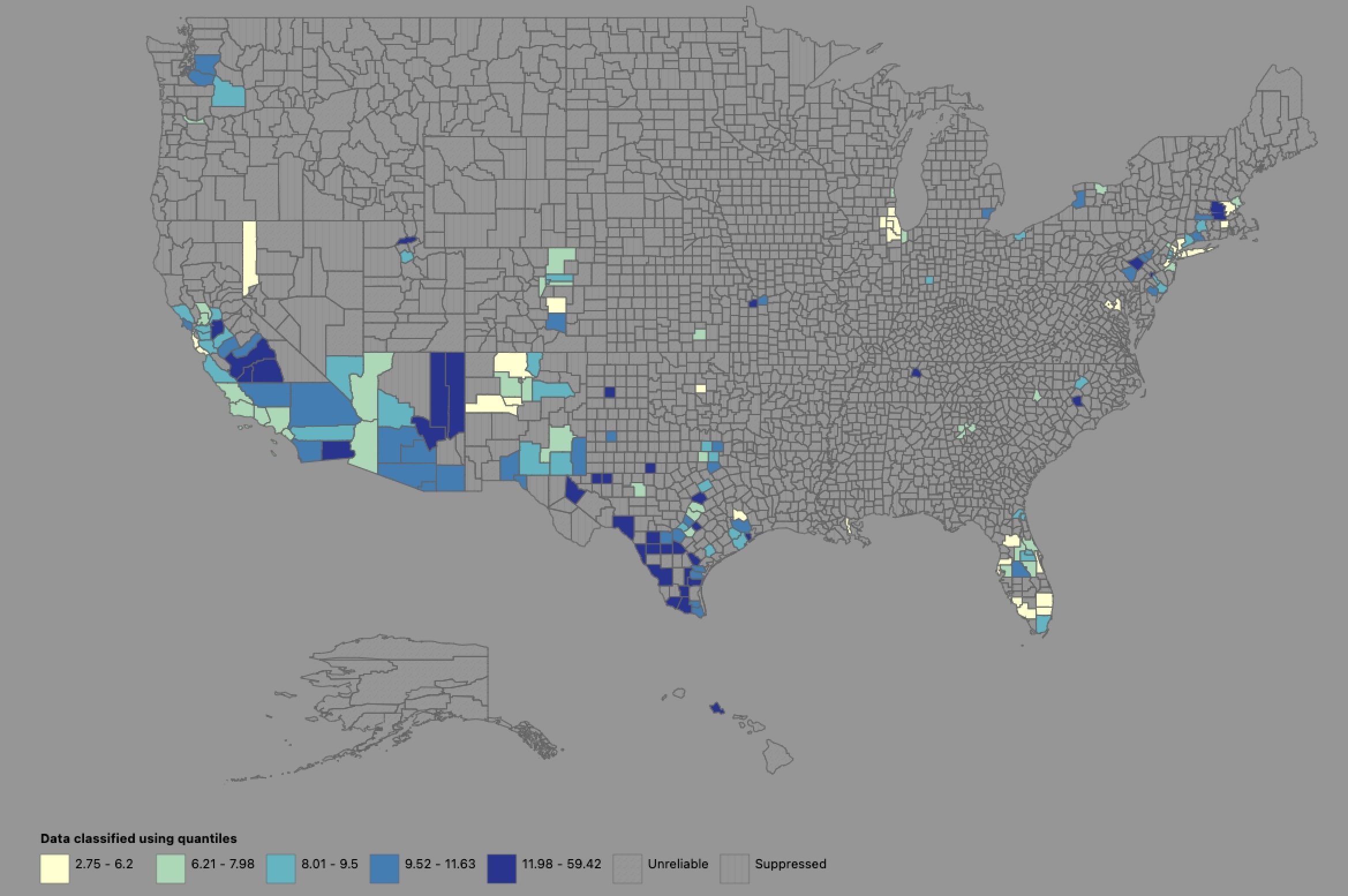
We identified 22,051 CS deaths nationally. AAMRs increased stepwise from Q1 to Q4 for API [7.2 to 9], Black [12.1 to 14.3], Hispanic [7.5 to 11.2], and White [8.9 to 11.5] populations; gradients were significant for Hispanics [F= 4.54, P =0.004] and Whites [F=13.2, P < 0.001] but not for Blacks or APIs. AIAN individuals experience uniformly high AAMRs with no SVI gradient [F= 0.04, P= 0.97]. Hotspots clustered in rural high-SVI counties of the South and Southwest: Russell County, AL [AAMR 149.1 for Blacks; 121.9 for Whites], Carter County, OK [69.1 for AIAN], and Navajo/Apache Counties, AZ [59.44 Hispanics].
Conclusions
County-level social vulnerability intensifies CS mortality for most racial groups, with steep gradients among Hispanic and White populations, while AIAN communities face persistently high risk irrespective of SVI. Race-SVI hotspot mapping pinpoints rural Southern and Southwestern counties where equitable access to timely revascularization, advanced heart failure therapies, and community-based prevention should be prioritized.
Cardiogenic shock [CS] remains highly lethal. Whether county-level structural vulnerabilities, as captured by the CDC Social Vulnerability Index [SVI], modify racial mortality gaps is unknown.
Objective
To quantify area-specific CS mortality gradients across SVI quartiles and to map high-burden hotspots.
Methods
We extracted mortality data about CS from CDC WONDER [2016–2020] and merged it with 2020 CDC SVI data. Age-adjusted mortality rates [AAMRs, per 100,000] were calculated for American Indian/Alaska Native [AIAN], Asian/Pacific Islander [API], Black, Hispanic, and White populations stratified by SVI quartile [Q1 being least, Q4 being most vulnerable]. One-way ANOVA tested AAMR differences across quartiles [alpha equal to 0.05]. Counties in Q4 whose race-specific AAMR exceeded the 95th percentile were designated hotspots.
Results
We identified 22,051 CS deaths nationally. AAMRs increased stepwise from Q1 to Q4 for API [7.2 to 9], Black [12.1 to 14.3], Hispanic [7.5 to 11.2], and White [8.9 to 11.5] populations; gradients were significant for Hispanics [F= 4.54, P =0.004] and Whites [F=13.2, P < 0.001] but not for Blacks or APIs. AIAN individuals experience uniformly high AAMRs with no SVI gradient [F= 0.04, P= 0.97]. Hotspots clustered in rural high-SVI counties of the South and Southwest: Russell County, AL [AAMR 149.1 for Blacks; 121.9 for Whites], Carter County, OK [69.1 for AIAN], and Navajo/Apache Counties, AZ [59.44 Hispanics].
Conclusions
County-level social vulnerability intensifies CS mortality for most racial groups, with steep gradients among Hispanic and White populations, while AIAN communities face persistently high risk irrespective of SVI. Race-SVI hotspot mapping pinpoints rural Southern and Southwestern counties where equitable access to timely revascularization, advanced heart failure therapies, and community-based prevention should be prioritized.
More abstracts on this topic:
3-Minute Heart Health App: A Feasibility Study
Abdulkarim Iya, Metzger Joseph, Stovitz Steven, Van't Hof Jeremy
Danish Pragmatic Randomized Trial to Evaluate the Effect of HeartLogic-Guided Management on Heart Failure Outcomes – The DANLOGIC-HF Preliminary Registry FindingsWitten Davodian Lise, Chien Christopher, Fudim Marat, Hernandez Adrian, Kwan Brian, Stolen Craig, Biering-soerensen Tor, Dyrby Johansen Niklas, Sattler Stefan Michael, Wolsk Emil, Risum Niels, Kober Lars, Gustafsson Finn, Davodian Danny, Solomon Scott