Final ID: MP1417
Association Between Creatinine-to-Cystatin C Ratio, Subclinical Myocardial Injury, and Mortality: National Health and Nutrition Examination Survey
Abstract Body (Do not enter title and authors here): Background: The creatinine-to-cystatin C ratio (CCR) is an emerging biomarker of skeletal muscle health that predicts cardiovascular outcomes. Subclinical myocardial injury (SCMI) affects over 20% of adults and increases mortality risk. The relationship between CCR, SCMI, and mortality remains unexplored.
Hypothesis: We hypothesized that: 1) Lower CCR would be associated with increased SCMI prevalence; 2) Both low CCR and SCMI would independently predict all-cause and cardiovascular disease (CVD) mortality; and 3) Participants with concurrent low CCR and SCMI would demonstrate the highest mortality risk.
Methods: We analyzed NHANES III (1988-1994) participants aged ≥40 years who underwent electrocardiogram (ECG) recording, excluding those with CVD history, ECG evidence of myocardial infarction, estimated glomerular filtration rate (eGFR) <30 mL/min/1.73m2, or missing data. CCR was calculated as serum creatinine (mg/dL)/cystatin C (mg/L) x 100. SCMI was defined as a cardiac infarction injury score ≥10 on 12-lead ECG. Mortality was ascertained from the National Death Index. Multivariable logistic regression assessed the baseline cross-sectional association between CCR (z-score standardized) and the presence of SCMI. Cox Proportional Hazard models were used to examine the association of combined CCR and SCMI categories with mortality (low CCR: lowest tertile <101.9; high CCR: upper two tertiles ≥101.9). Models were adjusted for age, sex, race/ethnicity, education, smoking, physical activity, body mass index, systolic blood pressure, anti-hypertensive medications, total and HDL cholesterol, lipid-lowering medications, and eGFR.
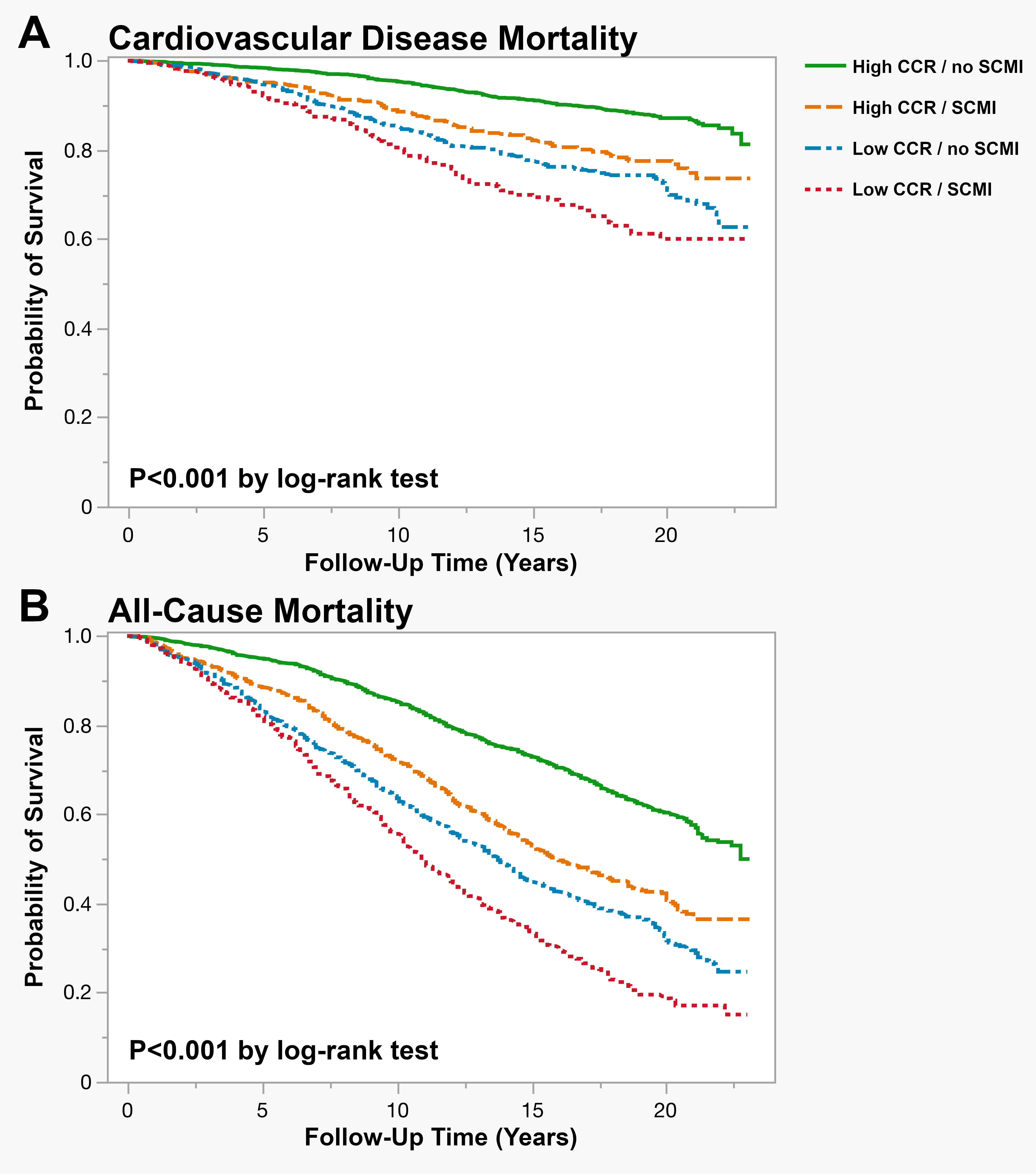
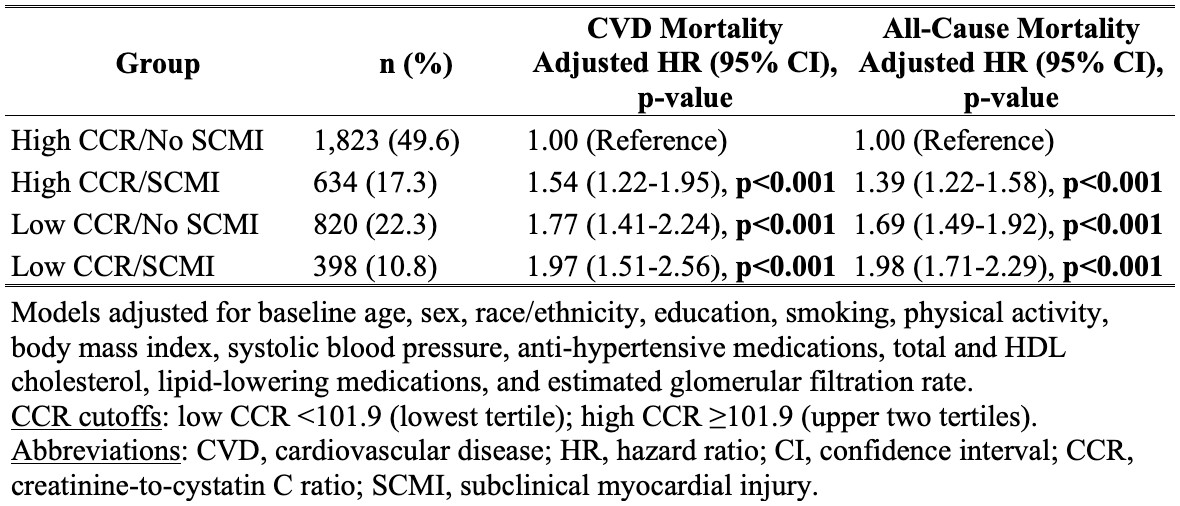
Results: Among 3,675 participants (mean age 64.8±12.4 years, 52.7% female), 1,032 (28.1%) had SCMI. Each 1-SD decrease in CCR was associated with 13% increased odds of SCMI (adjusted OR 1.13, 95% CI 1.02-1.25). During a median follow-up of 17.5 (9.9-19.6) years, 596 CVD deaths and 1,973 all-cause deaths occurred. Combined CCR-SCMI categories showed graded associations with mortality (Figure), with low CCR/SCMI showing the highest risk for both CVD mortality (adjusted HR 1.97, 95% CI 1.51-2.56) and all-cause mortality (adjusted HR 1.98, 95% CI 1.71-2.29) compared to high CCR/no SCMI (Table).
Conclusions: Low CCR is associated with increased SCMI prevalence. They both independently predict mortality, with the combination showing the greatest risk.
Hypothesis: We hypothesized that: 1) Lower CCR would be associated with increased SCMI prevalence; 2) Both low CCR and SCMI would independently predict all-cause and cardiovascular disease (CVD) mortality; and 3) Participants with concurrent low CCR and SCMI would demonstrate the highest mortality risk.
Methods: We analyzed NHANES III (1988-1994) participants aged ≥40 years who underwent electrocardiogram (ECG) recording, excluding those with CVD history, ECG evidence of myocardial infarction, estimated glomerular filtration rate (eGFR) <30 mL/min/1.73m2, or missing data. CCR was calculated as serum creatinine (mg/dL)/cystatin C (mg/L) x 100. SCMI was defined as a cardiac infarction injury score ≥10 on 12-lead ECG. Mortality was ascertained from the National Death Index. Multivariable logistic regression assessed the baseline cross-sectional association between CCR (z-score standardized) and the presence of SCMI. Cox Proportional Hazard models were used to examine the association of combined CCR and SCMI categories with mortality (low CCR: lowest tertile <101.9; high CCR: upper two tertiles ≥101.9). Models were adjusted for age, sex, race/ethnicity, education, smoking, physical activity, body mass index, systolic blood pressure, anti-hypertensive medications, total and HDL cholesterol, lipid-lowering medications, and eGFR.
Results: Among 3,675 participants (mean age 64.8±12.4 years, 52.7% female), 1,032 (28.1%) had SCMI. Each 1-SD decrease in CCR was associated with 13% increased odds of SCMI (adjusted OR 1.13, 95% CI 1.02-1.25). During a median follow-up of 17.5 (9.9-19.6) years, 596 CVD deaths and 1,973 all-cause deaths occurred. Combined CCR-SCMI categories showed graded associations with mortality (Figure), with low CCR/SCMI showing the highest risk for both CVD mortality (adjusted HR 1.97, 95% CI 1.51-2.56) and all-cause mortality (adjusted HR 1.98, 95% CI 1.71-2.29) compared to high CCR/no SCMI (Table).
Conclusions: Low CCR is associated with increased SCMI prevalence. They both independently predict mortality, with the combination showing the greatest risk.
More abstracts on this topic:
A Systematic Review and Network Meta-Analysis of Metastatic Castrate-Resistant Prostate Cancer Therapy Cardiotoxicity Given Metastatic Hormone-Sensitive Prostate Cancer Treatment History
Aziz Moez, Swaby Justin, Deng Brett, Hartshorne Taylor, Desai Shubh, Zhang Allan, Xiao Daniel, Sanchez Darren, Imber Jared, Song Jeffrey, Rivas Alexis, Molony Donald, Guhan Maya, Ranganath Shreyas, Jacob Jerril, Ziaolhagh Ali, Ali Abdelrahman, Yusuf Syed, Canfield Steven, Iliescu Cezar, Monlezun Dominique, Higgason Noel, Brunckhorst Oliver, Roland Jerry, Owen Christopher, Iacobucci Alexander Samuel, Galan Jacob
4D Flow MRI Evaluation of Cardiovascular Risk-Related Alterations in Heart-Brain Hemodynamics in Cognitively Healthy Aging AdultsNajafi Anahita, Rogalski Emily, Jarvis Kelly, Richter Adam, Lytchakov Anna, Benson Theresa, Jin Ning, Davids Rachel, Schnell Susanne, Ragin Ann, Weintraub Sandra