Final ID: MP96
Intensive Systolic Blood Pressure Lowering Reduces Cardiovascular Events in Hypertensive Adults Regardless of Metabolic Health Status: Insights from SPRINT
Abstract Body (Do not enter title and authors here): Background: Hypertension often coexists with metabolic abnormalities that increase cardiovascular disease (CVD) risk. While intensive systolic blood pressure (SBP) lowering reduces cardiovascular events, it is unclear whether this benefit varies by metabolic health status in primary prevention.
Objective: To examine whether metabolic health modifies the effect of standard (<140 mmHg) versus intensive (<120 mmHg) SBP lowering on CVD risk in adults in the Systolic Blood Pressure Intervention Trial (SPRINT).
Methods: We included 7,454 SPRINT participants without baseline CVD and with complete metabolic health and outcome data. Metabolic health was defined using modified metabolic syndrome criteria: triglycerides ≥150 mg/dL, high-density lipoprotein cholesterol <40 mg/dL (men) or <50 mg/dL (women), glucose ≥100 mg/dL, and body mass index ≥30 kg/m2 (used in place of waist circumference due to data availability). Individuals with ≤1 abnormality were classified as metabolically healthy (MH) and those with ≥2 as metabolically unhealthy (MUH). The primary outcome was a composite of myocardial infarction, acute coronary syndrome, stroke, heart failure, or CVD death. Cox proportional hazards models were adjusted for covariates listed in the Table.
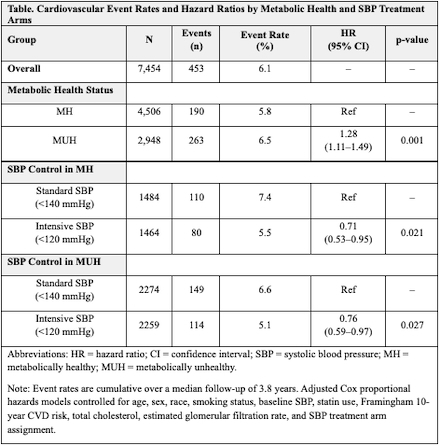
Results: Of 7,454 participants (mean age 67 years, 37.6% female), 2,948 (39.6%) were classified as MUH. Treatment arms were balanced within MH and MUH groups. Over a median follow-up of 3.8 years, 453 CVD events occurred, with a higher event rate in the MUH group compared to the MH group (6.5% vs. 5.8%). MUH group had a higher risk of CVD (HR 1.28; 95% CI 1.11–1.49; p=0.001) compared to the MH group. Intensive SBP lowering reduced CVD risk by 29% in MH (HR 0.71; 95% CI 0.53–0.95; ARR 1.9%; NNT ≈53) and by 24% in MUH (HR 0.76; 95% CI 0.59–0.97; ARR 1.5%; NNT ≈67) (Table). Multiplicative interaction term assessing effect modification between SBP treatment arm and metabolic health was not statistically significant (p=0.77).
Conclusions: In hypertensive adults without diabetes, unfavorable metabolic health was associated with a higher risk of incident CVD events. While absolute risk was greater in MUH individuals, both MH and MUH groups experienced significant relative risk reductions with intensive SBP lowering. Despite no significant interaction, intensive SBP lowering was associated with reduced CVD risk in both groups. These findings support intensive SBP treatment to reduce CVD risk regardless of metabolic health status.
Objective: To examine whether metabolic health modifies the effect of standard (<140 mmHg) versus intensive (<120 mmHg) SBP lowering on CVD risk in adults in the Systolic Blood Pressure Intervention Trial (SPRINT).
Methods: We included 7,454 SPRINT participants without baseline CVD and with complete metabolic health and outcome data. Metabolic health was defined using modified metabolic syndrome criteria: triglycerides ≥150 mg/dL, high-density lipoprotein cholesterol <40 mg/dL (men) or <50 mg/dL (women), glucose ≥100 mg/dL, and body mass index ≥30 kg/m2 (used in place of waist circumference due to data availability). Individuals with ≤1 abnormality were classified as metabolically healthy (MH) and those with ≥2 as metabolically unhealthy (MUH). The primary outcome was a composite of myocardial infarction, acute coronary syndrome, stroke, heart failure, or CVD death. Cox proportional hazards models were adjusted for covariates listed in the Table.
Results: Of 7,454 participants (mean age 67 years, 37.6% female), 2,948 (39.6%) were classified as MUH. Treatment arms were balanced within MH and MUH groups. Over a median follow-up of 3.8 years, 453 CVD events occurred, with a higher event rate in the MUH group compared to the MH group (6.5% vs. 5.8%). MUH group had a higher risk of CVD (HR 1.28; 95% CI 1.11–1.49; p=0.001) compared to the MH group. Intensive SBP lowering reduced CVD risk by 29% in MH (HR 0.71; 95% CI 0.53–0.95; ARR 1.9%; NNT ≈53) and by 24% in MUH (HR 0.76; 95% CI 0.59–0.97; ARR 1.5%; NNT ≈67) (Table). Multiplicative interaction term assessing effect modification between SBP treatment arm and metabolic health was not statistically significant (p=0.77).
Conclusions: In hypertensive adults without diabetes, unfavorable metabolic health was associated with a higher risk of incident CVD events. While absolute risk was greater in MUH individuals, both MH and MUH groups experienced significant relative risk reductions with intensive SBP lowering. Despite no significant interaction, intensive SBP lowering was associated with reduced CVD risk in both groups. These findings support intensive SBP treatment to reduce CVD risk regardless of metabolic health status.
More abstracts on this topic:
A peptoid derivative of alpha-calcitonin gene related peptide improves cardiac function in pressure-overload heart failure mice
Kumar Ambrish, Deloach Sarah, Dipette Donald, Potts Jay
2-Methoxyestradiol By Inhibiting Central Action of 12S-Hydroxyeicosatetraenoic Acid Protects Ovariectomized Mice From HypertensionDutta Shubha, Singh Purnima, Song Chi Young, Shin Ji Soo, Malik Kafait