Final ID: MP582
Patterns and Correlates of Heart Rate Among US Adults in the All of Us Research Program
Abstract Body (Do not enter title and authors here): Background: Heart rate is a core component of clinical assessment in patients with cardiovascular disease. However, single-point measurements of heart rate during clinical encounters do not fully capture its dynamic variability in living environments. Advances in wearable technology provide an opportunity to assess patterns of heart rate at scale.
Aims: To assess patterns of heart rate and its clinical and sociodemographic correlates among US adults.
Methods: Participants in the All of Us Research Program (AoU) who were 18 years of age or older and had available wearable data between 2018-2023 were included. We assessed diurnal patterns of mean heart rate and conducted sensitivity analyses across key clinical and demographic subgroups and state of residence. Correlation of heart rate with prevalent diseases was assessed in a phenome-wide association study (PheWAS).
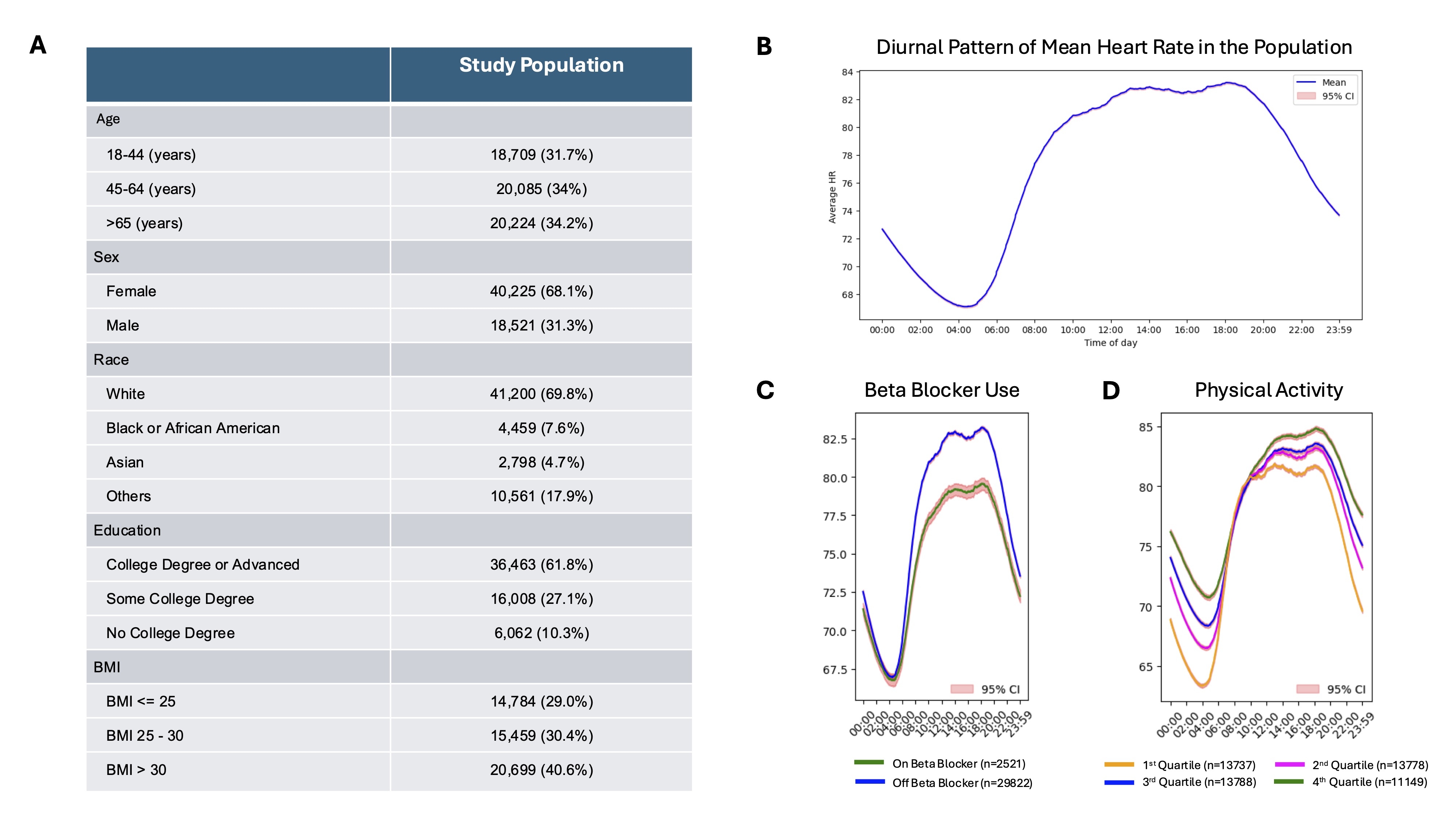
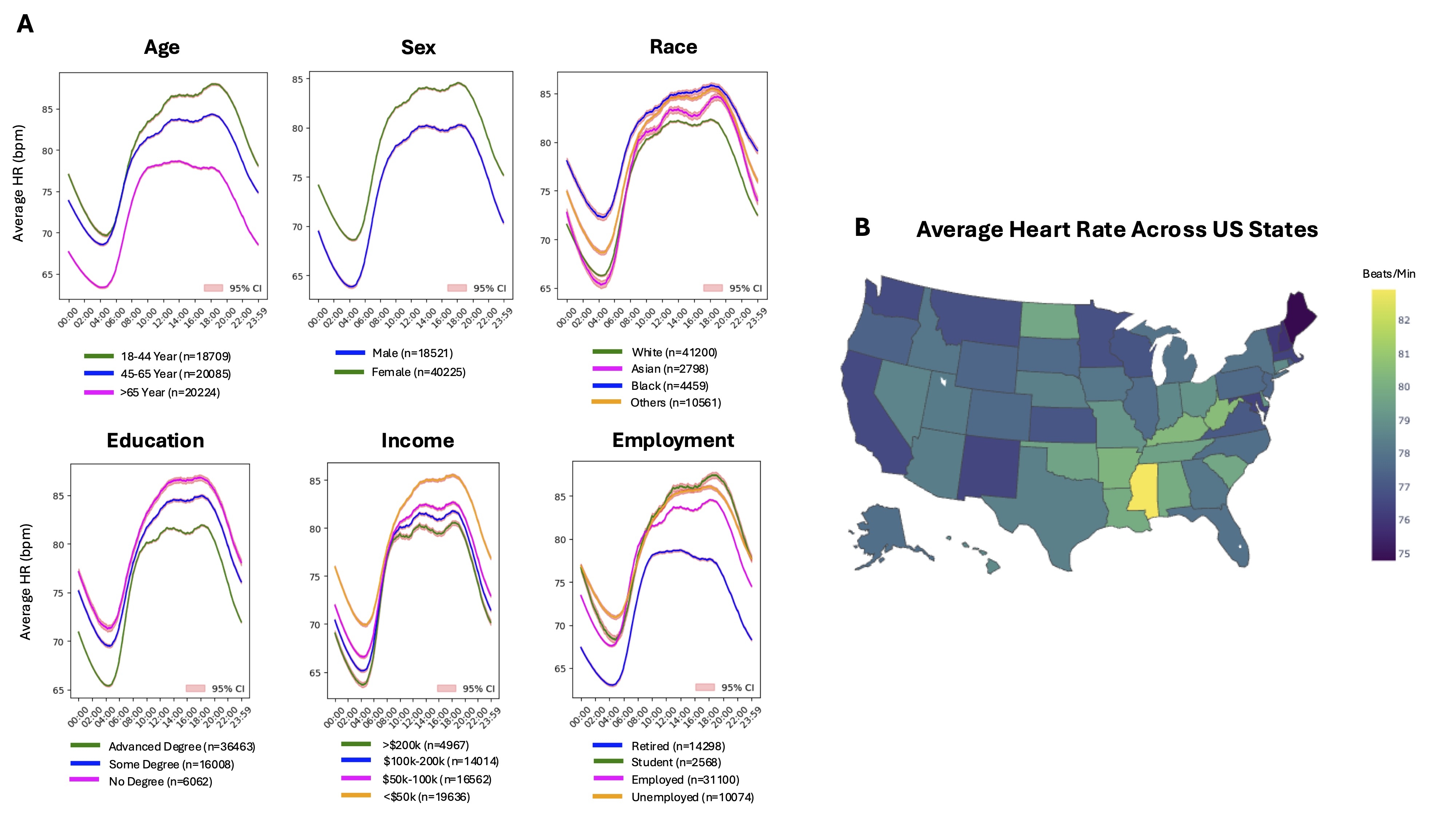
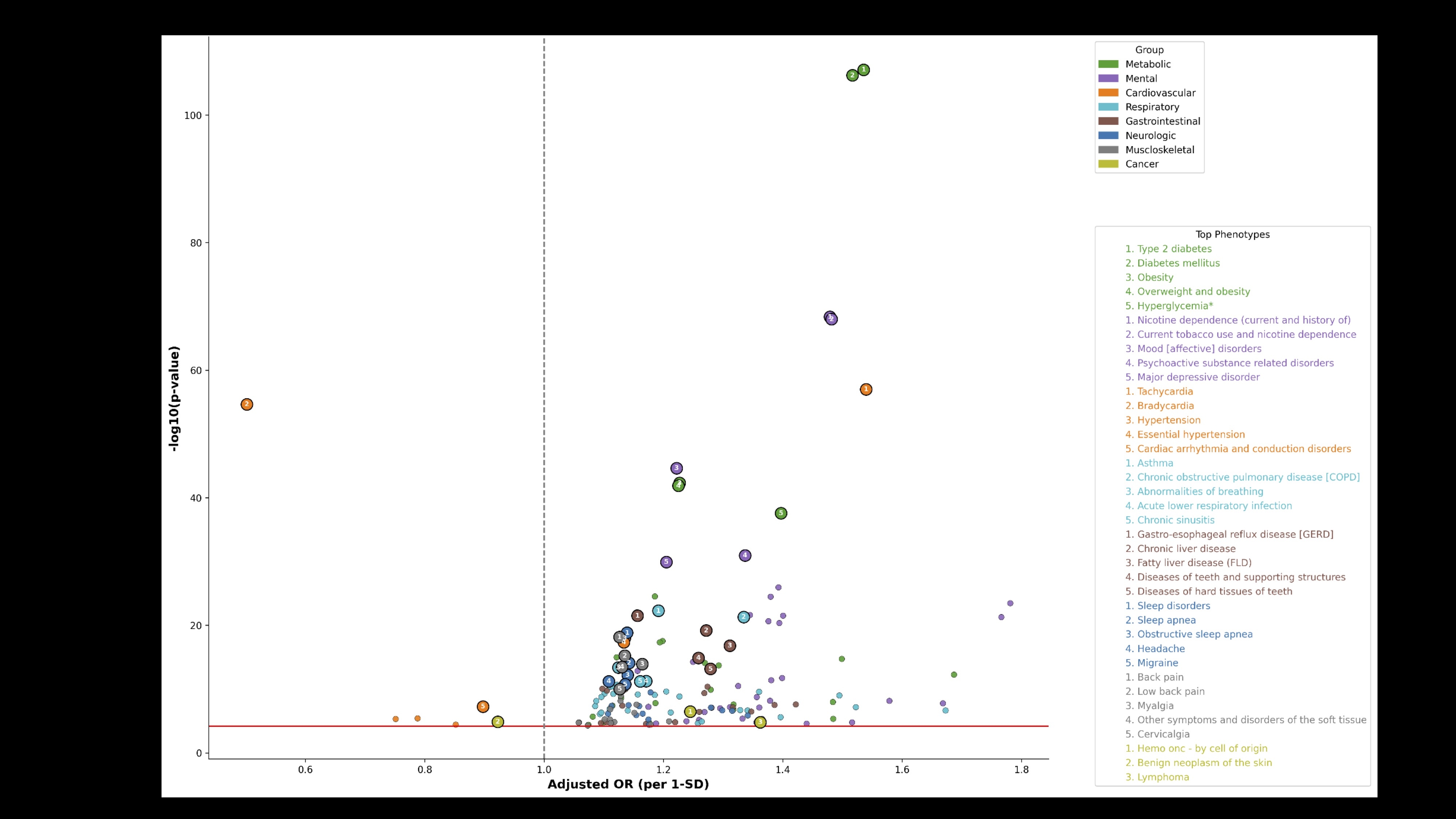
Results: A total of 59,018 participants (68% female, 70% white, median age 55 [IQR 40-66] years, Figure 1A) with 16,260,167 person-days of heart rate monitoring over median follow up of 18 months were included. Mean heart rate showed a circadian pattern with peak value of 83 bpm at 6:05 pm and trough value of 67 bpm at 4:23 am (Figure 1B). The diurnal range of heart rate decreased from 16 bpm in the study population to 12 bpm in those receiving a beta-blocker (HRPeak 79 bpm and HRTrough 67 bpm), and increased to 19 bpm in individuals in the highest quartile of step count (HRPeak 82 bpm and HRTrough 63 bpm, Figure 1C-D). Participants who were 65 years of age or older, retired, male, white, with college or advanced degrees, and income > $200k had lower heart rates compared to other subgroups (p<0.001 for all, Figure 2A). Residents of Northeast, Midwest, and West Coast had lower heart rates than those living in Central South (Figure 2B). In PheWAS (n=32,972), higher heart rate was most strongly associated with cardiometabolic risk factors such as obesity (OR 1.23 [95%CI 1.19-1.26]), and tobacco use (OR 1.48 [1.42-1.55]) and nicotine dependence (OR 1.47 [1.42-1.54]) after adjustment for age, sex, and race (Figure 3).
Conclusions: Wearable monitoring in the nationwide cohort of AoU uncovers distinct patterns of heart rate variation across sociodemographic subgroups and geographic regions. Longitudinal measurement of heart rate unlocks new opportunities to assess the complex interaction of societal and biological factors and their impacts on cardiovascular health.
Aims: To assess patterns of heart rate and its clinical and sociodemographic correlates among US adults.
Methods: Participants in the All of Us Research Program (AoU) who were 18 years of age or older and had available wearable data between 2018-2023 were included. We assessed diurnal patterns of mean heart rate and conducted sensitivity analyses across key clinical and demographic subgroups and state of residence. Correlation of heart rate with prevalent diseases was assessed in a phenome-wide association study (PheWAS).
Results: A total of 59,018 participants (68% female, 70% white, median age 55 [IQR 40-66] years, Figure 1A) with 16,260,167 person-days of heart rate monitoring over median follow up of 18 months were included. Mean heart rate showed a circadian pattern with peak value of 83 bpm at 6:05 pm and trough value of 67 bpm at 4:23 am (Figure 1B). The diurnal range of heart rate decreased from 16 bpm in the study population to 12 bpm in those receiving a beta-blocker (HRPeak 79 bpm and HRTrough 67 bpm), and increased to 19 bpm in individuals in the highest quartile of step count (HRPeak 82 bpm and HRTrough 63 bpm, Figure 1C-D). Participants who were 65 years of age or older, retired, male, white, with college or advanced degrees, and income > $200k had lower heart rates compared to other subgroups (p<0.001 for all, Figure 2A). Residents of Northeast, Midwest, and West Coast had lower heart rates than those living in Central South (Figure 2B). In PheWAS (n=32,972), higher heart rate was most strongly associated with cardiometabolic risk factors such as obesity (OR 1.23 [95%CI 1.19-1.26]), and tobacco use (OR 1.48 [1.42-1.55]) and nicotine dependence (OR 1.47 [1.42-1.54]) after adjustment for age, sex, and race (Figure 3).
Conclusions: Wearable monitoring in the nationwide cohort of AoU uncovers distinct patterns of heart rate variation across sociodemographic subgroups and geographic regions. Longitudinal measurement of heart rate unlocks new opportunities to assess the complex interaction of societal and biological factors and their impacts on cardiovascular health.
More abstracts on this topic:
Autonomic inflexibility in Response to Mental Stress in Women with Coronary Microvascular Dysfunction: A Pilot Study
Huang Jingwen, Mcclellan Olivia, Ibrahim Rand, Sterling Trevor, Rashid Fauzia, Shah Amit, Murtala Abdulkareem, Bremner James Douglas, Vaccarino Viola, Quyyumi Arshed, Mehta Puja, Sheikh Shafa-at, Dave Esha, Thaker Vishrut, Ahmed Taha, Harris Kristen, Medina-inojosa Jose, Hashmi Hania, Evenhuis Bernard
A Novel Composite Artificial Intelligence-Electrocardiography Risk Score Is Independently Associated with Mortality in Chronic Tricuspid RegurgitationCiobanu Andrea, Pellikka Patricia, Kane Garvan, Pislaru Sorin, Anand Vidhu, Naser Jwan, Wood Julia, Friedman Paul, Vinereanu Dragos, Nkomo Vuyisile, Pislaru Cristina, Lara-breitinger Kyla, Thaden Jeremy