Final ID: EPI8
Association between Household Sleep Environment and Sleep Health Characteristics in Middle-Aged Adults: The Coronary Artery Risk Development in Young Adults (CARDIA)—Sleep Study
Hypothesis: Individuals with adverse HHSE will have poorer sleep health.
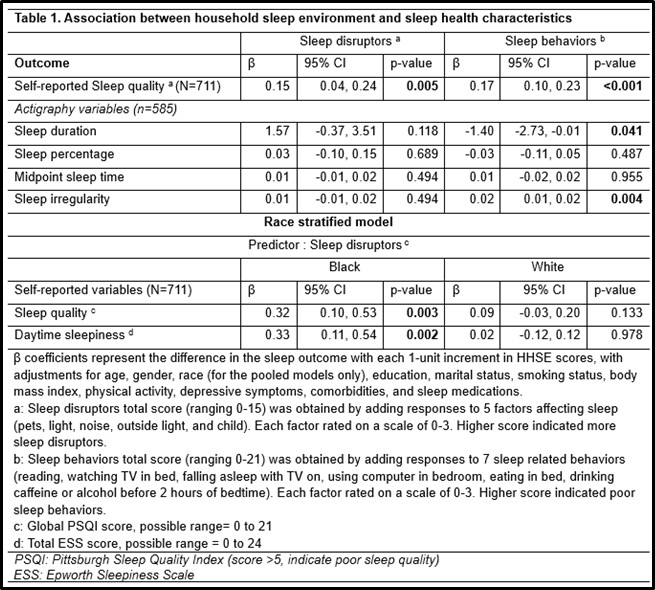
Methods: We used cross-sectional data from the CARDIA sleep ancillary study at Year 35. HHSE was assessed in two domains (i.e., sleep disruptors and sleep behaviors) using a self-reported questionnaire (see Table footnote).The HHSE domain scores were derived from questionnaire responses, and a higher score indicated more sleep disruptors or poorer sleep behaviors. Sleep outcomes were: 1) sleep quality assessed with the Pittsburgh Sleep Quality Index (PSQI) and daytime sleepiness assessed with the Epworth Sleepiness Scale (ESS) and 2) actigraphy-measured sleep duration, sleep percentage, midpoint sleep time, and sleep regularity. Robust regression estimated differences in sleep outcomes corresponding to each 1-unit increment in HHSE. Covariates were adjusted as appropriate (Table 1). Racial differences in associations of interest were examined by testing for interaction
Results: Participants’ mean age was 61.5 years, 63% were women, and 36.7% were Black. Medians (IQR) of PSQI, ESS scores, sleep duration, sleep percentage, midpoint sleep time, and sleep regularity were: 5 (4, 8), 5 (3, 7), 6.9 hours (IQR= 6.3, 7.5), 91% (IQR= 88, 93.4), 2:54 AM (IQR= 2:18, 3:42), and 0.7 hours (IQR= 0.5, 1.2), respectively. After multivariable adjustment, both more sleep disruptors and poor sleep behaviors were associated with self-reported poor sleep quality. Poor sleep behaviors were associated with actigraphy-measured shorter sleep duration and sleep irregularity. HHSE showed no association with sleep percentage and midpoint sleep time (Table 1). In stratified analysis, more sleep disruptors were associated with self-reported poor sleep quality (p-interaction= 0.027) and greater daytime sleepiness (p-interaction= 0.019) only in Black participants.
Conclusions: Adverse household sleep environment was related to subjective poor sleep quality and to objective shorter sleep duration and sleep irregularity. Future studies should investigate reasons why Black adults appear more susceptible to household sleep disruptors. Interventions to mitigate sleep disruptors and promote healthy sleep practices may help to improve sleep health.
More abstracts on this topic:
Siegler James, Aboul-nour Hassan, De Havenon Adam, Culbertson Collin, Melkumova Emiliya, Jillella Dinesh, Dumitrascu Oana, Doolittle Charles, Yahnke Ian, Sathya Anvitha, Brown Samantha, Penckofer Mary, Kang Jieun, Bowman Anna, Brorson James, Shahrivari Mahan, Elangovan Cheran, Sloane Kelly, Alvi Muhammad, Krishnaiah Balaji, Kam Wayneho, Farooqui Mudassir, Badillo Goicoechea Elena, Nahab Fadi, Rojas-soto Diana, Sharma Richa, Thottempudi Neeharika, Nedelcu Simona, Smith Matthew, Herpich Franziska, Glover Patrick, Chahien Dalia, Sehgal Siddharth, Eklund Kelsey, Liebeskind David, Linares Guillermo, Daniel Jean-philippe, Al Kasab Sami, Singh Eesha, D'souza Marissa, Gaudio Elizabeth, Aziz Yasmin, Yaghi Shadi, Salehi Omran Setareh, Stretz Christoph, Thon Jesse, Lineback Christina, Khasiyev Farid, Kerrigan Deborah, Ali Hamid
Association of Body Size and Shape Metrics with Atherosclerotic Cardiovascular Disease and Mortality: Ethnic Differences in a Nationally Representative Cohort of U.S. AdultsMangalesh Sridhar, Shah Priyansh, Chi Kuan Yu, Nouri Armin, Rossi Raiza, Borkowski Pawel, Faillace Robert, Nanna Michael