Final ID: MP1514
Atrial Fibrillation Risk Estimated Using Electrocardiogram-based Artificial Intelligence Stratifies Incidence of Atrial Fibrillation-Related Stroke and Heart Failure
Abstract Body (Do not enter title and authors here): Background: Risk of future atrial fibrillation (AF) can be estimated using artificial intelligence (AI)-enabled electrocardiogram (ECG) analysis. However, it remains unknown whether such models may also enrich for risk of potentially preventable AF-related adverse outcomes (e.g., stroke, heart failure [HF]).
Hypothesis: We hypothesized that AF risk estimates derived from a validated ECG-based AI model would also associate with future incidence of stroke and HF.
Methods: Among primary care and cardiology patients at two institutions (Massachusetts General Hospital [MGH] and Brigham and Women's Hospital [BWH]) separate from model development, we estimated 5-year AF risk using ECG-AI, a previously validated ECG-based deep learning model developed to predict future AF risk. We assessed associations between estimated AF risk and incident AF, stroke, and HF using Cox proportional hazards models adjusted for age and sex. We fit analogous models for AF-related stroke and HF, defined as incident stroke or HF in which AF occurred either before the event or within 30 days after the event. Individuals with either AF or the target outcome at baseline were excluded. Event discrimination was quantified using the area under the time-dependent receiver operating characteristic curves (AUROC) at 5 years. Cumulative risk of events was plotted across tertiles of ECG-AI risk score.
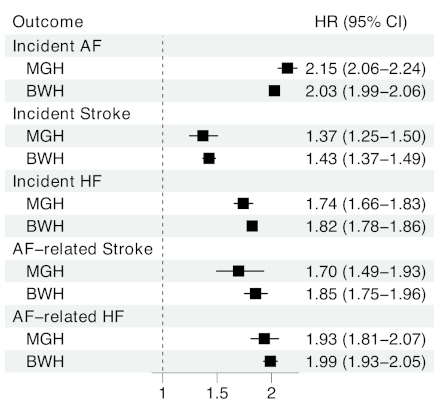
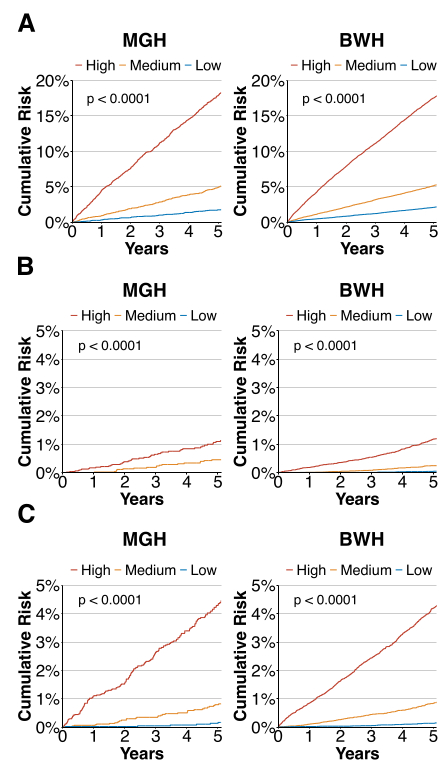
Results: We identified 15,269 patients from MGH (mean age 56.5±16.6 years, 48.6% women, median follow-up period 8.3 years [Q1–Q3: 3.4–14.3]) and 73,080 from BWH (56.5±16.0, 54.7%, 7.5 [Q1–Q3: 3.0–12.6]). Across both institutions, there were a total of 12,168 AF events, 1,010 AF-related stroke events, and 2,935 AF-related HF events over the follow-up period (Table 1). A higher ECG-AI risk score was independently associated with higher hazard for all outcomes (Figure 1), and stratified the longitudinal risk of all outcomes (Figure 2). For AF-related stroke, AUROC was 0.788 (95% confidence interval [CI] 0.743–0.835) at MGH and 0.815 (95% CI 0.791–0.843) at BWH. For AF-related HF, AUROC was 0.838 (95% CI 0.813–0.862) at MGH and 0.836 (95% CI 0.823–0.847) at BWH.
Conclusion: An ECG-based AI model developed to predict incident AF also demonstrates potential to identify individuals at high risk of AF-related stroke and HF. Future work is warranted to investigate whether targeted preventive measures (e.g., AF screening) guided by ECG-based AI may reduce AF-related morbidity.
Hypothesis: We hypothesized that AF risk estimates derived from a validated ECG-based AI model would also associate with future incidence of stroke and HF.
Methods: Among primary care and cardiology patients at two institutions (Massachusetts General Hospital [MGH] and Brigham and Women's Hospital [BWH]) separate from model development, we estimated 5-year AF risk using ECG-AI, a previously validated ECG-based deep learning model developed to predict future AF risk. We assessed associations between estimated AF risk and incident AF, stroke, and HF using Cox proportional hazards models adjusted for age and sex. We fit analogous models for AF-related stroke and HF, defined as incident stroke or HF in which AF occurred either before the event or within 30 days after the event. Individuals with either AF or the target outcome at baseline were excluded. Event discrimination was quantified using the area under the time-dependent receiver operating characteristic curves (AUROC) at 5 years. Cumulative risk of events was plotted across tertiles of ECG-AI risk score.
Results: We identified 15,269 patients from MGH (mean age 56.5±16.6 years, 48.6% women, median follow-up period 8.3 years [Q1–Q3: 3.4–14.3]) and 73,080 from BWH (56.5±16.0, 54.7%, 7.5 [Q1–Q3: 3.0–12.6]). Across both institutions, there were a total of 12,168 AF events, 1,010 AF-related stroke events, and 2,935 AF-related HF events over the follow-up period (Table 1). A higher ECG-AI risk score was independently associated with higher hazard for all outcomes (Figure 1), and stratified the longitudinal risk of all outcomes (Figure 2). For AF-related stroke, AUROC was 0.788 (95% confidence interval [CI] 0.743–0.835) at MGH and 0.815 (95% CI 0.791–0.843) at BWH. For AF-related HF, AUROC was 0.838 (95% CI 0.813–0.862) at MGH and 0.836 (95% CI 0.823–0.847) at BWH.
Conclusion: An ECG-based AI model developed to predict incident AF also demonstrates potential to identify individuals at high risk of AF-related stroke and HF. Future work is warranted to investigate whether targeted preventive measures (e.g., AF screening) guided by ECG-based AI may reduce AF-related morbidity.
More abstracts on this topic:
Anatomic Physiological Scoring is a Comparable Predictor of Adult Congenital Operative Morbidity and Mortality
La Brenda, Taylor-fishwick Jon, Macbeth Morgan, Soohoo Megan
Agency Epinephrine Dosing Intervals and Patient Characteristics in Out-of-Hospital Cardiac Arrest: A National EMS StudyDefilippo Michael, Braude Darren, Root Christopher, Covert Harold, Fisher Benjamin, Huebinger Ryan