Final ID: MP1952
Redefining Vasoplegia: A New Hemodynamic Model for Differentiating Cardiac vs Vascular Dysfunction using the Resistance Flow Ratio
Abstract Body (Do not enter title and authors here): Background: Traditional definitions of vasoplegia, based on fixed thresholds of mean arterial pressure (MAP), cardiac index (CI), and systemic vascular resistance (SVR), fail to account for hemodynamic interdependencies. Such definitions overlook compensated states, ignore mixed etiologies with simultaneous cardiac and vascular dysfunction, omit body surface area covariation and inadequately assess true organ perfusion pressure. This study introduces a new hemodynamic model based on the Resistance Flow Ratio (RFR), defined as the ratio of SVR index (SVRI) to CI. We use this ratio to differentiate cardiac versus vascular dysfunction and to identify early compensated states that occur before the transition to overt clinical decompensation.
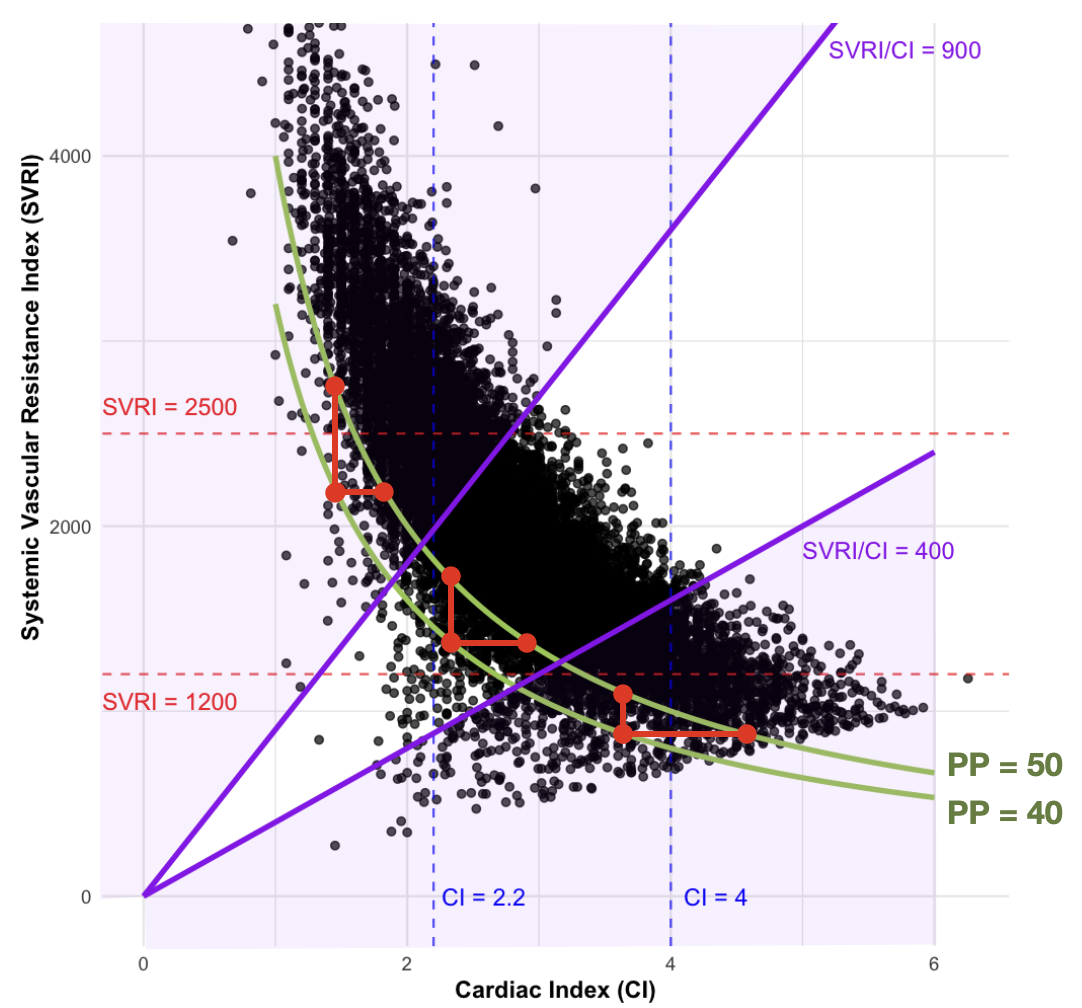
Methods: We retrospectively analyzed postoperative hemodynamic data from 3,393 cardiac surgical patients monitored with pulmonary artery catheters between 2014 and 2024. Patients were categorized into three distinct groups based on the RFR: 1) predominantly cardiac dysfunction, 2) predominantly vascular dysfunction, and 3) mixed dysfunction. Perfusion pressure (PP = MAP–CVP) was used to determine compensation status, with a PP>50 mmHg considered compensated. The minimum independent change in SVRI or CI required to increase PP by 10 mmHg was calculated to determine the optimal RFR thresholds for differentiating between cardiac and vascular dysfunction.
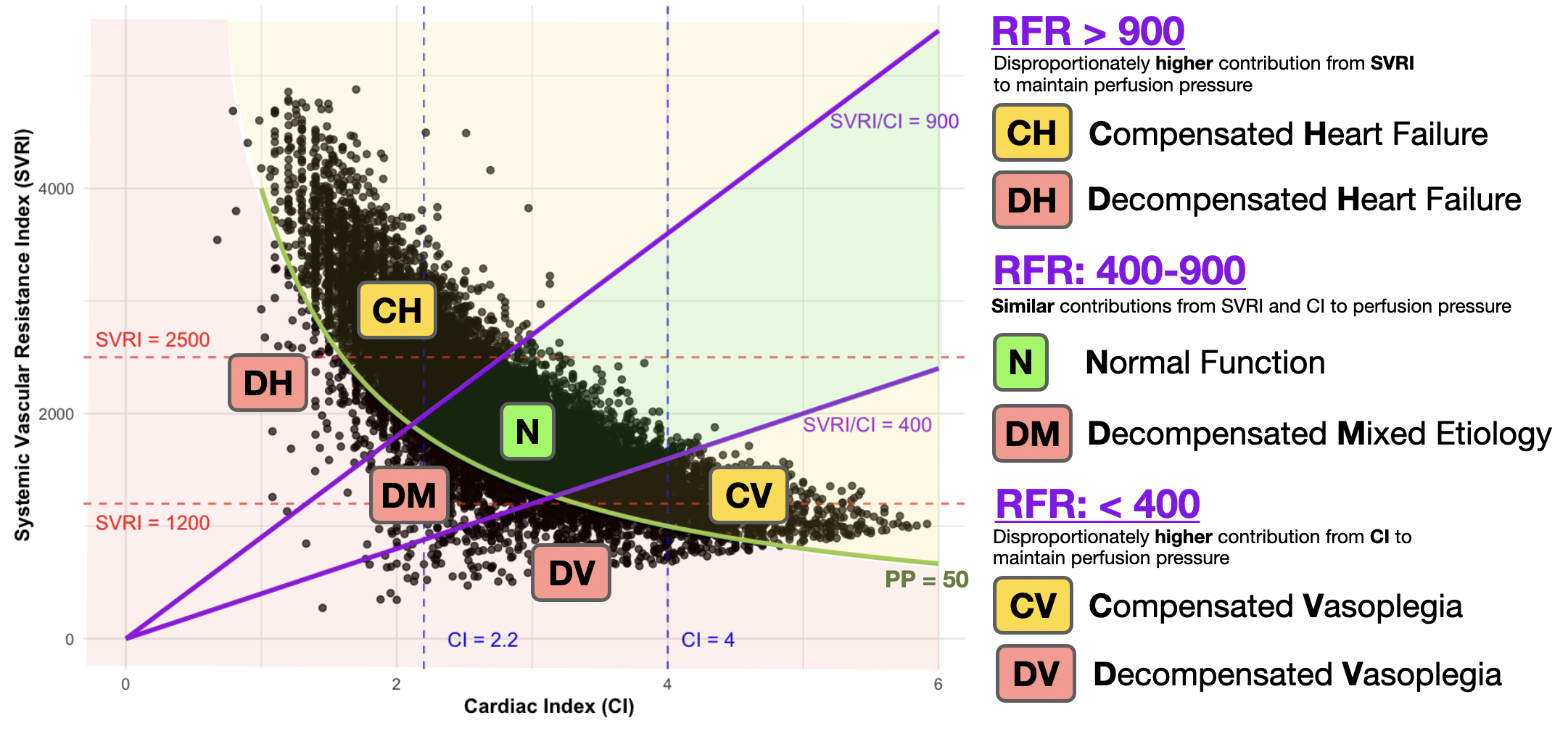
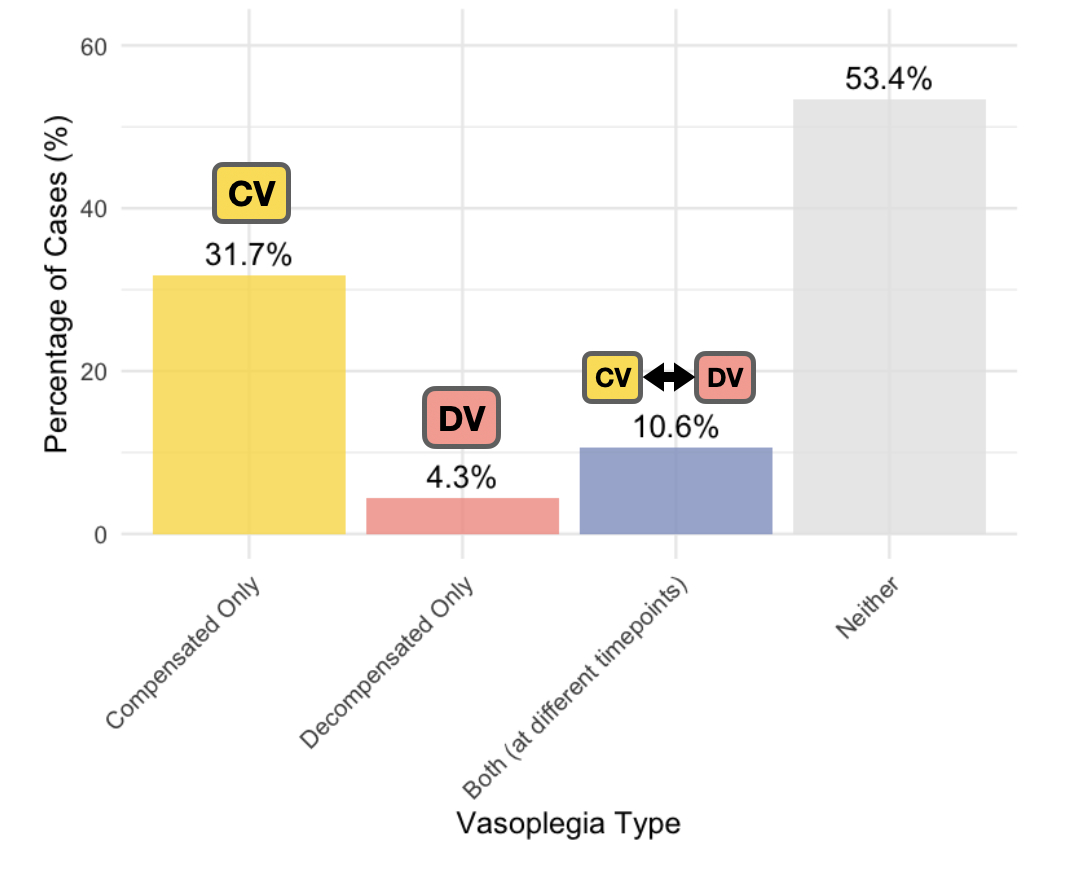
Results: Identified thresholds were as follows: at RFR >900, increasing cardiac output was ≥1.5x more efficient at increasing PP, whereas at RFR <400, vasoconstriction was ≥1.5x more effective. Six distinct hemodynamic states were identified: 1) compensated heart failure (RFR>900, PP>50), 2) decompensated heart failure (RFR>900, PP<50), 3) normal function (RFR 400–900, PP>50), 4) mixed decompensation (RFR 400–900, PP<50), 5) compensated vasoplegia (RFR<400, PP>50), and 6) decompensated vasoplegia (RFR<400, PP<50). Among the analyzed cohort, compensated vasoplegia occurred in 31.7%, decompensated vasoplegia alone in 4.3%, and both compensated and decompensated vasoplegia in 10.6%.
Conclusions: Resistance Flow Ratio provides improved differentiation between cardiac and vascular dysfunction, identifying compensated states otherwise missed by traditional definitions. This novel approach has the potential to enhance clinical management through earlier postoperative recognition of distinct forms of hemodynamic deterioration, enabling more targeted therapeutic interventions.
Methods: We retrospectively analyzed postoperative hemodynamic data from 3,393 cardiac surgical patients monitored with pulmonary artery catheters between 2014 and 2024. Patients were categorized into three distinct groups based on the RFR: 1) predominantly cardiac dysfunction, 2) predominantly vascular dysfunction, and 3) mixed dysfunction. Perfusion pressure (PP = MAP–CVP) was used to determine compensation status, with a PP>50 mmHg considered compensated. The minimum independent change in SVRI or CI required to increase PP by 10 mmHg was calculated to determine the optimal RFR thresholds for differentiating between cardiac and vascular dysfunction.
Results: Identified thresholds were as follows: at RFR >900, increasing cardiac output was ≥1.5x more efficient at increasing PP, whereas at RFR <400, vasoconstriction was ≥1.5x more effective. Six distinct hemodynamic states were identified: 1) compensated heart failure (RFR>900, PP>50), 2) decompensated heart failure (RFR>900, PP<50), 3) normal function (RFR 400–900, PP>50), 4) mixed decompensation (RFR 400–900, PP<50), 5) compensated vasoplegia (RFR<400, PP>50), and 6) decompensated vasoplegia (RFR<400, PP<50). Among the analyzed cohort, compensated vasoplegia occurred in 31.7%, decompensated vasoplegia alone in 4.3%, and both compensated and decompensated vasoplegia in 10.6%.
Conclusions: Resistance Flow Ratio provides improved differentiation between cardiac and vascular dysfunction, identifying compensated states otherwise missed by traditional definitions. This novel approach has the potential to enhance clinical management through earlier postoperative recognition of distinct forms of hemodynamic deterioration, enabling more targeted therapeutic interventions.
More abstracts on this topic:
Abatacept Drug-Induced Loeffler Endocarditis: A Manifestation of Hypereosinophilic Syndrome
Sweeting Alexander, Atalay Michael, Agarwal Saurabh, Hulten Edward, Patel Yash
Association Between Liberal Fluid Strategy and Postoperative Outcomes in Cardiac Surgery: A Systematic Review and Bayesian Meta-AnalysisHortêncio Melo Rafael, Cappellaro Anelise, Almeida Luiz, Gomez Victor