Final ID: Su2012
Machine Learning to Identify Vasoplegia without a Pulmonary Artery Catheter using the Resistance Flow Ratio
Abstract Body (Do not enter title and authors here): Introduction: Postoperative vasoplegia is a complex syndrome, with traditional definitions unable to differentiate isolated vascular dysfunction and mixed cardiogenic-vasoplegic states. We previously developed a novel model of vasoplegia based on the Resistance Flow Ratio (RFR), defined as the ratio of systemic vascular resistance index (SVRI) to cardiac index (CI). This study used machine learning to predict RFR identified vasoplegia using only routinely available hemodynamic parameters, without using pulmonary artery (PA) catheter derived data.
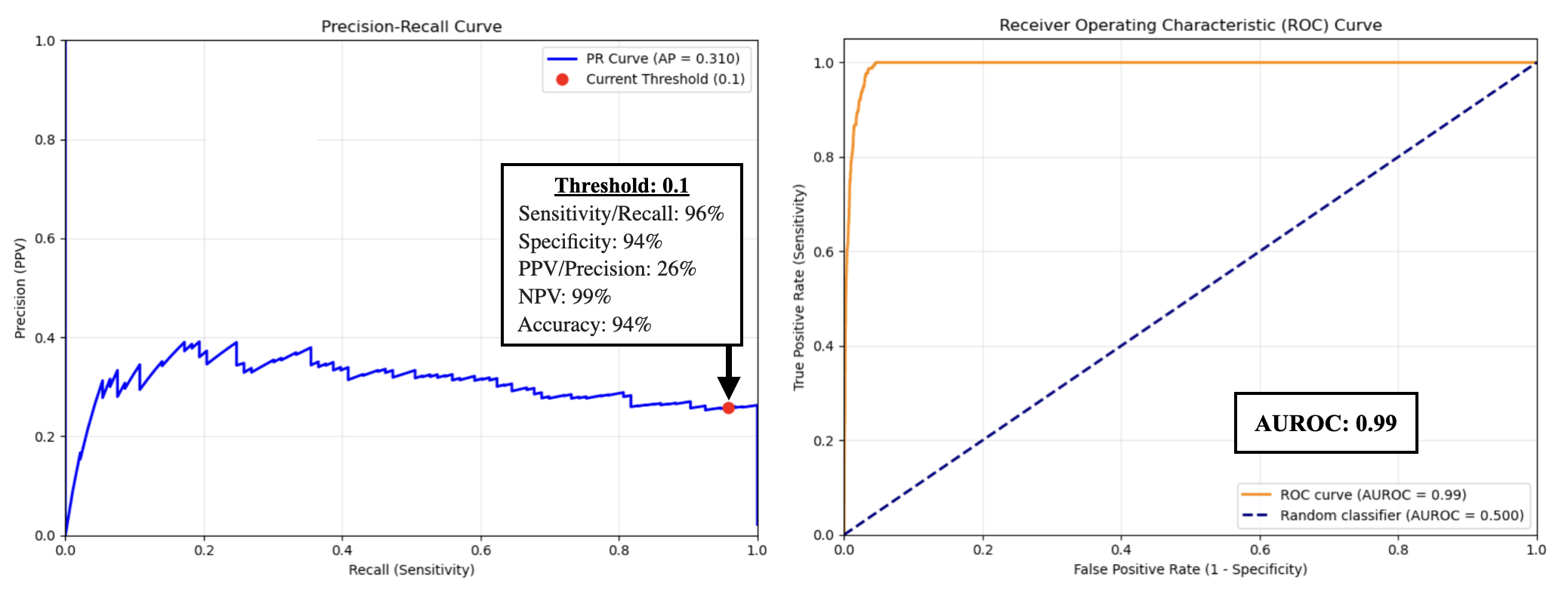
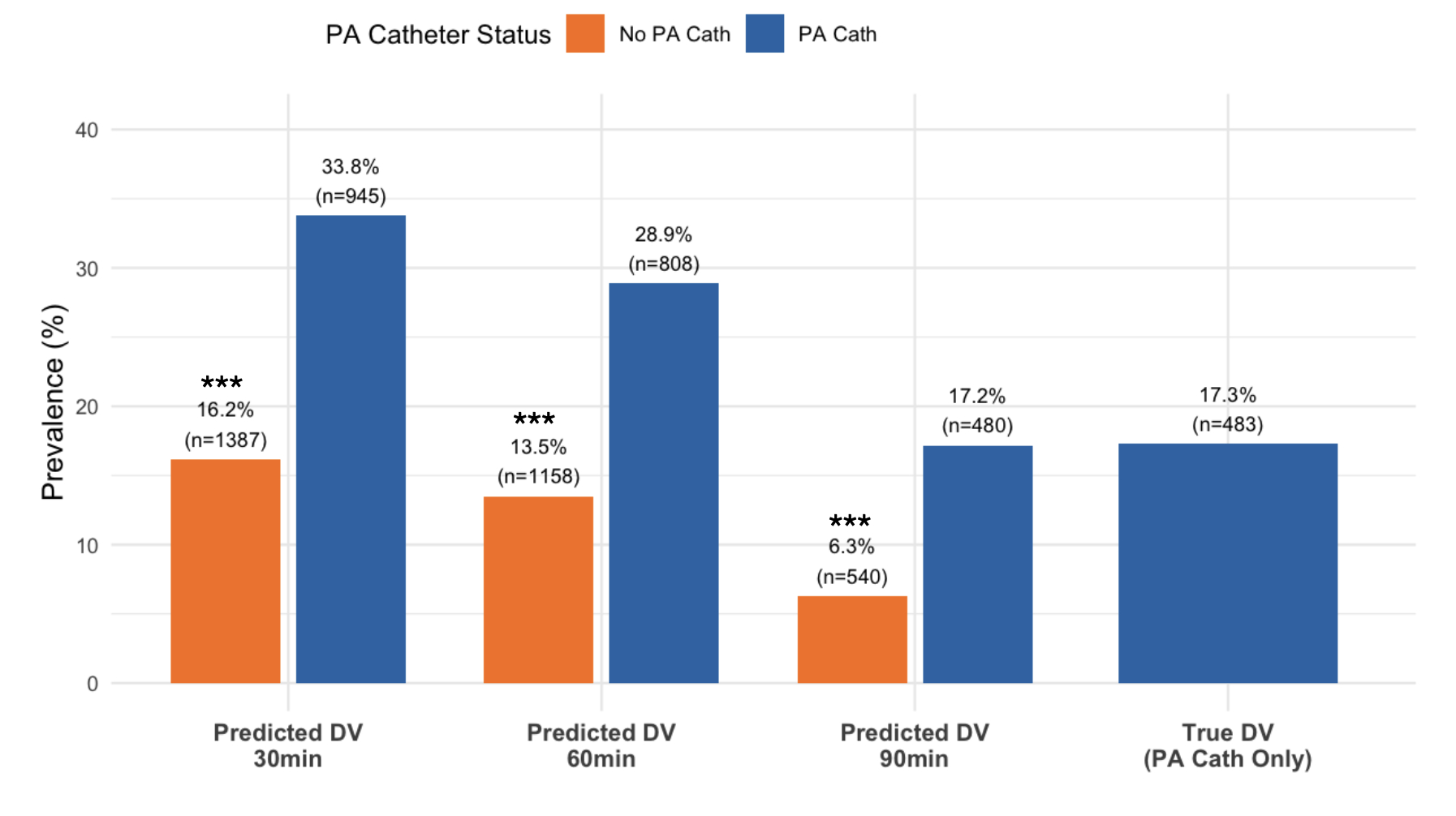
Methods: We retrospectively analyzed postoperative hemodynamic data from 11,365 cardiac surgical patients monitored with and without PA catheters between 2014-2024. Decompensated Vasoplegia (DV) was defined as a RFR<400 and perfusion pressure <50 mmHg. An XGBoost model was trained using four input variables: heart rate, diastolic blood pressure, pulse pressure, and central venous pressure. To incorporate time-dependent hemodynamic patterns, a second model was trained using data from three timepoints: the index measurement and two prior timepoints separated by >10 minutes, with <3 hours between the first and last. The cohort was split 80:20 into training and testing sets. Performance was evaluated using area under the receiver operating characteristic curve (AUROC), precision-recall curve (AUPRC), sensitivity, specificity, and positive predictive value (PPV) at multiple thresholds. The model was backtested on the full dataset to assess DV prevalence at 30-,60-,and 90-minute intervals.
Results: Among all cases, 3,393 had sufficient PA catheter data to calculate RFR. DV occurred in 14.9%. On the test set, the AUROC of the single timepoint model was 0.98 and AUPRC 0.31, reflecting inherent class imbalance. At a threshold of 0.1, the model identified DV with 96% sensitivity, 94% specificity, and 26% PPV. Adding prior timepoints did not improve performance over the single-timepoint model. When applied to patients without a PA catheter, 16% were predicted to have DV for > 30 min, 14% for > 60 min, and 6% for 90 min. Predicted DV prevalence was significantly lower in non-PA catheter patients across all time intervals. (p < 0.05).
Conclusions: A machine learning model trained on non-invasive hemodynamic parameters adequately predicts vasoplegia as defined by our RFR-based framework. This approach enables identification of without PA catheterization, offering a physiologically grounded alternative to legacy definitions.
Methods: We retrospectively analyzed postoperative hemodynamic data from 11,365 cardiac surgical patients monitored with and without PA catheters between 2014-2024. Decompensated Vasoplegia (DV) was defined as a RFR<400 and perfusion pressure <50 mmHg. An XGBoost model was trained using four input variables: heart rate, diastolic blood pressure, pulse pressure, and central venous pressure. To incorporate time-dependent hemodynamic patterns, a second model was trained using data from three timepoints: the index measurement and two prior timepoints separated by >10 minutes, with <3 hours between the first and last. The cohort was split 80:20 into training and testing sets. Performance was evaluated using area under the receiver operating characteristic curve (AUROC), precision-recall curve (AUPRC), sensitivity, specificity, and positive predictive value (PPV) at multiple thresholds. The model was backtested on the full dataset to assess DV prevalence at 30-,60-,and 90-minute intervals.
Results: Among all cases, 3,393 had sufficient PA catheter data to calculate RFR. DV occurred in 14.9%. On the test set, the AUROC of the single timepoint model was 0.98 and AUPRC 0.31, reflecting inherent class imbalance. At a threshold of 0.1, the model identified DV with 96% sensitivity, 94% specificity, and 26% PPV. Adding prior timepoints did not improve performance over the single-timepoint model. When applied to patients without a PA catheter, 16% were predicted to have DV for > 30 min, 14% for > 60 min, and 6% for 90 min. Predicted DV prevalence was significantly lower in non-PA catheter patients across all time intervals. (p < 0.05).
Conclusions: A machine learning model trained on non-invasive hemodynamic parameters adequately predicts vasoplegia as defined by our RFR-based framework. This approach enables identification of without PA catheterization, offering a physiologically grounded alternative to legacy definitions.
More abstracts on this topic:
Analysis of Ventricular Fibrillation Waveform Response to Asphyxial Hemodynamics in an Infant Swine Model of Out-of-Hospital Cardiac Arrest
Jackson Aaron, Gumucio Jorge, Menegazzi James, Salcido David
A Novel Cardiac Simulator "ped UT-Heart" to Support Decision-Making in Surgical Procedures for Complex Congenital Heart DiseaseShiraishi Isao, Kurosaki Kenichi, Iwai Shigemitsu, Washio Takumi, Sugiura Seiryo, Hisada Toshiaki