Final ID: MP2697
Coronary Microvascular Disease Modulates Long-Term Outcomes in Myocardial Infarction with Non-Obstructive Coronary Arteries
Abstract Body (Do not enter title and authors here): Background: Coronary microvascular dysfunction (CMD) is a common cause of angina with non-obstructive coronary arteries (ANOCA), but its role in patients with a history of myocardial infarction with non-obstructive coronary arteries (MINOCA) is much less understood. We investigated the incidence of major adverse cardiac and cerebrovascular events (MACCE) in patients undergoing invasive assessment for CMD, divided into patients with MINOCA versus patients with ANOCA. We hypothesized that CMD would be common in both groups.
Methods: Serial patients undergoing invasive coronary provocation testing between 2012 and 2022 were divided into MINOCA (n=76) or ANOCA (n=561). Doppler study was performed in the left anterior descending artery. CMD was defined as either coronary flow reserve (CFR) <2.5 with adenosine or <50% increase in flow with acetylcholine. Patients were followed prospectively through 2025. Incidence of MACCE (cardiac death, non-fatal MI, hospitalization for heart failure, urgent revascularization, and stroke) was compared between MINOCA and ANOCA and further analyzed by CMD status. Kaplan-Meier curves were constructed and Cox proportional hazards models were used to estimate hazard ratios (HRs).
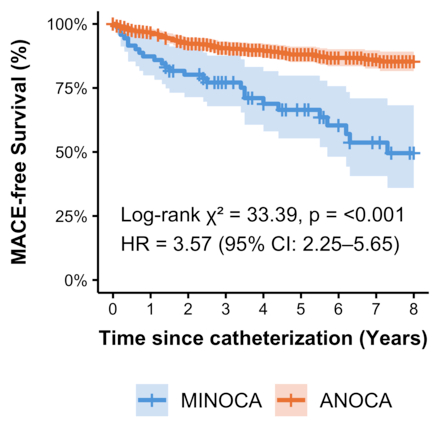
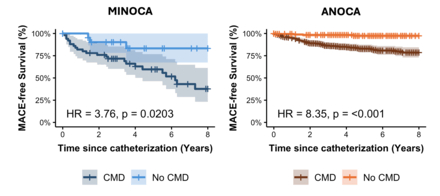
Results: Among patients with MINOCA, 53 of 76 (70%) had CMD, compared to 363 of 561 (65%) with ANOCA. Invasive provocation testing was performed a median of 163 days (IQR 13 – 255 days) after the MI in the MINOCA group. Patients were then followed for a median of 4.4 years (IQR 3.0 – 6.9 years). MACCE-free survival was significantly lower in patients with MINOCA compared to those with ANOCA (HR = 3.57, p < 0.001; Figure 1). The major contributor to MACCE was non-fatal MI in MINOCA (24%) and heart failure hospitalization in ANOCA (6%). The presence of CMD was associated with worse prognosis in both MINOCA (HR = 3.76, p = 0.02) and ANOCA (HR = 8.35, p < 0.001; Figure 2).
Conclusions: Patients with MINOCA experience significantly higher long-term risk of major adverse events compared to those with ANOCA. CMD is common in both groups and is independently associated with worse outcomes. Specifically, patients with CMD had higher rates of MACCE over time, regardless of whether they presented with MINOCA or ANOCA. Invasive assessment of CMD in patients with myocardial infarction and non-obstructive coronary arteries may improve risk stratification and inform management strategies in these understudied populations
Methods: Serial patients undergoing invasive coronary provocation testing between 2012 and 2022 were divided into MINOCA (n=76) or ANOCA (n=561). Doppler study was performed in the left anterior descending artery. CMD was defined as either coronary flow reserve (CFR) <2.5 with adenosine or <50% increase in flow with acetylcholine. Patients were followed prospectively through 2025. Incidence of MACCE (cardiac death, non-fatal MI, hospitalization for heart failure, urgent revascularization, and stroke) was compared between MINOCA and ANOCA and further analyzed by CMD status. Kaplan-Meier curves were constructed and Cox proportional hazards models were used to estimate hazard ratios (HRs).
Results: Among patients with MINOCA, 53 of 76 (70%) had CMD, compared to 363 of 561 (65%) with ANOCA. Invasive provocation testing was performed a median of 163 days (IQR 13 – 255 days) after the MI in the MINOCA group. Patients were then followed for a median of 4.4 years (IQR 3.0 – 6.9 years). MACCE-free survival was significantly lower in patients with MINOCA compared to those with ANOCA (HR = 3.57, p < 0.001; Figure 1). The major contributor to MACCE was non-fatal MI in MINOCA (24%) and heart failure hospitalization in ANOCA (6%). The presence of CMD was associated with worse prognosis in both MINOCA (HR = 3.76, p = 0.02) and ANOCA (HR = 8.35, p < 0.001; Figure 2).
Conclusions: Patients with MINOCA experience significantly higher long-term risk of major adverse events compared to those with ANOCA. CMD is common in both groups and is independently associated with worse outcomes. Specifically, patients with CMD had higher rates of MACCE over time, regardless of whether they presented with MINOCA or ANOCA. Invasive assessment of CMD in patients with myocardial infarction and non-obstructive coronary arteries may improve risk stratification and inform management strategies in these understudied populations
More abstracts on this topic:
A Novel Multivariate Scoring System for Diagnosing Post-Myocardial Infarction Pericarditis Following Percutaneous Coronary Intervention
Bolaji Olayiwola, Omoru Okiemute, Upreti Prakash, Echari Blanche, Shoar Saeed, Basit Jawad, Alraies M Chadi
Association of Blood Pressure Time in Target Range with Outcomes Among NIH "All of Us” CohortAgarwal Neel, St John Julie, Xlaffinx Xlukex