Final ID: 46
Rapid Implementation of Endovascular Thrombectomy Is Associated with Improved Health Equity in Stroke Outcomes: An Analysis of the Get With The Guidelines®-Stroke Registry
Methods: This was a retrospective, observational, cohort study in the American Heart Association’s Get With The Guidelines®-Stroke (GWTG-Stroke) Program based on two epochs: January 2010 to December 2014 and January 2016 to December 2019. From 2,272 hospitals in the United States, 173,049 patients who were potentially eligible for EVT were included. Our exposure was availability of EVT at system level defined by degree of implementation of EVT by each hospital after balancing key patient and hospital characteristics with overlap weighting. The primary endpoint was difference in in-hospital mortality for patients from ZIP codes with median income >$60,000 vs <$60,000. Secondary endpoints were differences in in-hospital mortality by race/ethnicity, sex, insurance status, county-level poverty, and county-level educational attainment, as well as differences in ambulatory status at hospital discharge and a composite of in-hospital mortality/discharge to hospice.
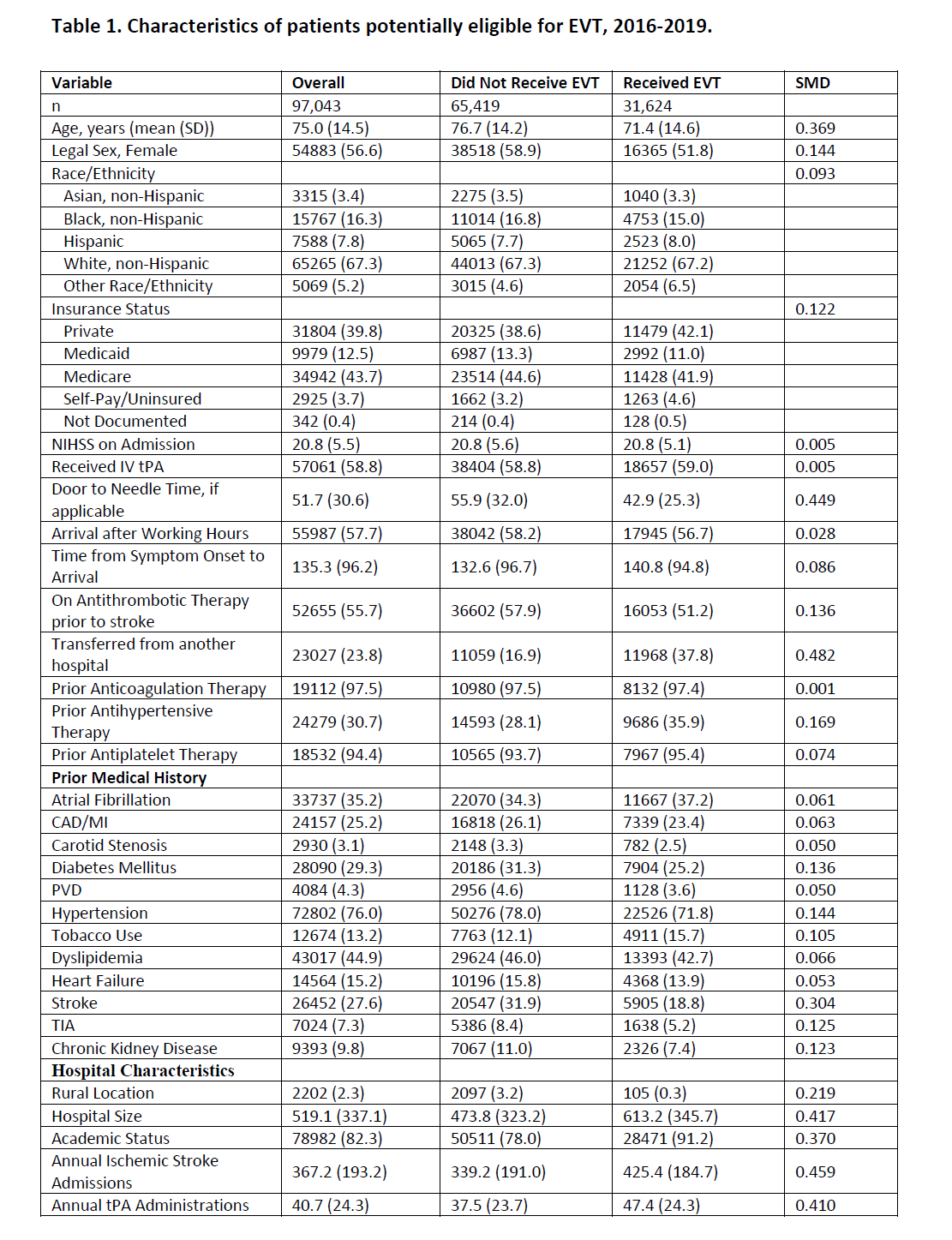
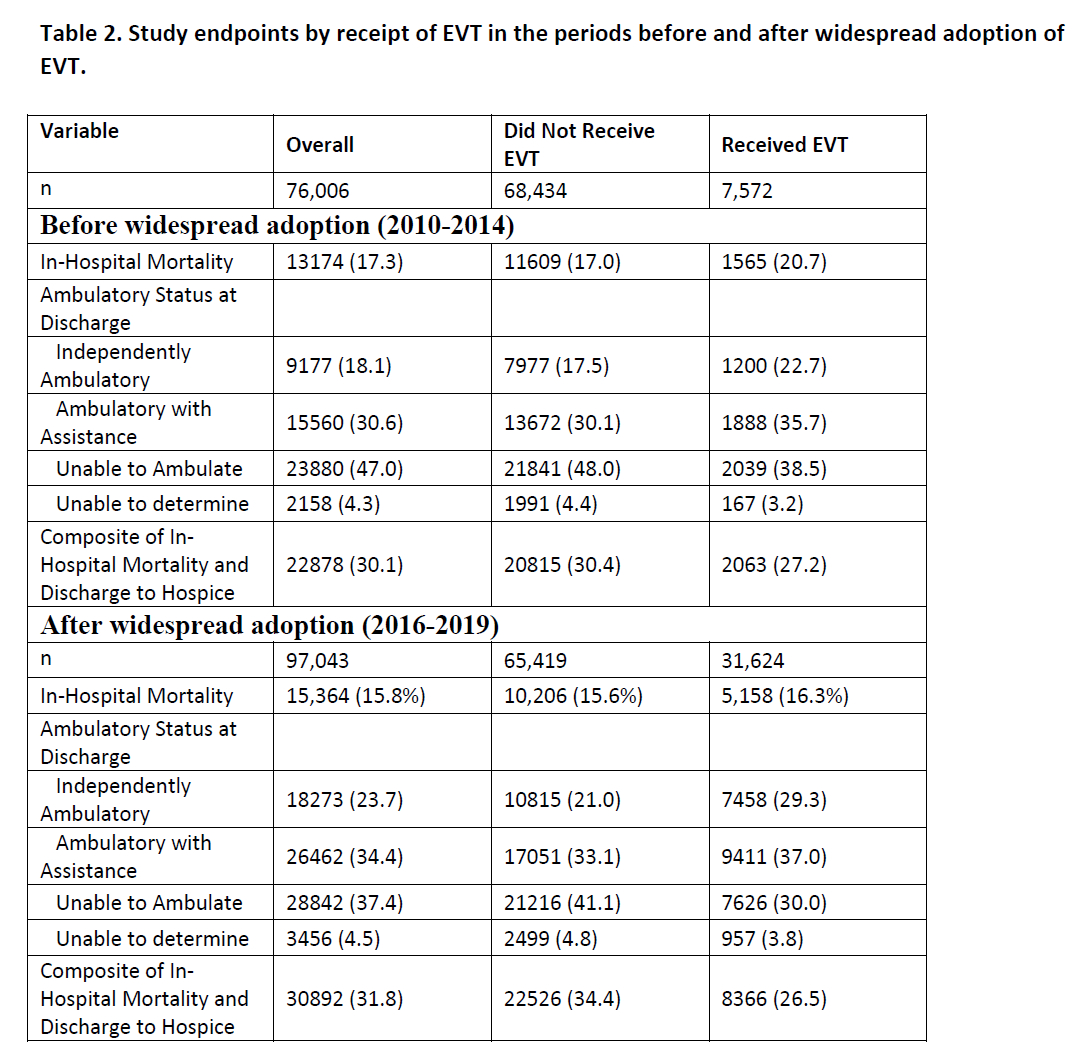
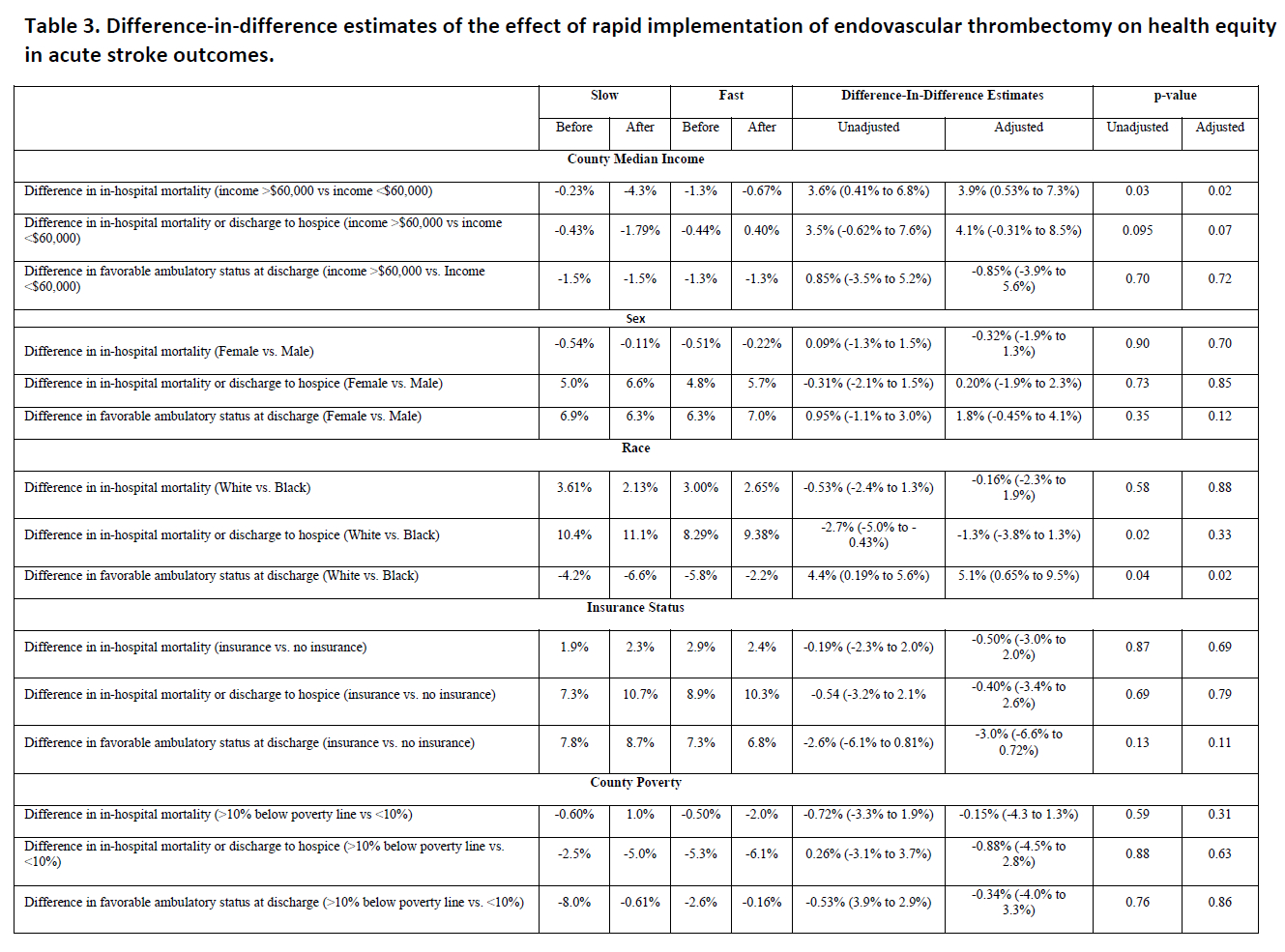
Results: Of 173,049 patients potentially eligible for EVT (median age 75; 53.9% female), 39,196 (22.7%) received EVT (7,572 [10.0% of potentially eligible patients] between 2010-2014 and 31,624 [32.6% of potentially eligible patients] between 2016-2019 (Table 1). In 2010-2014, 1,565 (20.7%) of patients and in 2016-2019 5,158 (16.3%) who received EVT died in-hospital (Table 2). For the primary endpoint and exposure, rapid implementation of EVT was associated with decreased disparities in mortality rates for patients from counties with median income >$60,000 versus <$60,000 (ARD 3.9%, 95% CI 0.53-7.3%, p=0.02). For secondary analyses, after overlap weighting, rapid implementation of EVT was not associated in changes in health equity in any endpoints by race/ethnicity, sex, county poverty rates, county educational attainment, or insurance status (Table 3).
Conclusions: Rapid implementation of EVT was associated with improvements in health equity by community median income and was not associated with new or worsening disparities in any health outcome by race/ethnicity, sex, insurance status, or other county-level socioeconomic markers.
More abstracts on this topic:
Maria Shannon, Mojares Joseph, Zrelak Patricia
Acute intracranial stenting among patients with large vessel occlusion: Clinical and radiological outcomes of the RESISTANT International registryRequena Manuel, Lopez-frias Alfonso, Hassan Ameer, Miller Samantha, Zapata-arriaza Elena, De Alboniga-chindurza Asier, Bergui Mauro, Molinaro Stefano, Sousa Joao Andre, Gomes Fábio, Alexandre Andrea, Olive-gadea Marta, Pedicelli Alessandro, Hofmeister Jeremy, Machi Paolo, Scarcia Luca, Kalsoum Erwah, Meira Torcato, Amorim José, Ortega-gutierrez Santiago, Rodriguez Aaron, Capasso Francesco, Kaesmacher Johannes, Renieri Leonardo, Romano Daniele, Barcena Eduardo, Abdalkader Mohamad, Perry Da Camara Catarina, Yavagal Dileep, Vega Pedro, Ozdemir Atilla Ozcan, Smajda Stanislas, Khalife Jane, Mujanovic Adnan, Biraschi Francesco, Castro Pedro, Siddiqui Adnan, Navia Pedro, Ntoulias Nikolaos, Velo Mariano, Zamarro Joaquin, Zaidat Osama, Sierra-gomez Alicia, Marto Joao Pedro, Geyik Serdar, Tomasello Alejandro, Senadim Songul, Cervo Amedeo, Salcuni Andrea, Moreu Manuel
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.