Final ID: WMP92
Assessing Effects of Intra-Arterial Verapamil on Cerebral Hemodynamics and Autoregulation Following Aneurysmal Subarachnoid Hemorrhage
Methods: We evaluated near-infrared spectroscopy (NIRS) and mean arterial pressure (MAP) recordings from aSAH patients who underwent angiography with infusion of IA verapamil for anterior circulation vasospasm. NIRS-derived regional oxygen saturation (rSO2) from the affected hemisphere was correlated with MAP to derive the optimal blood pressure (MAPOPT) at which cerebral autoregulation was the most preserved, as well as the associated lower and upper limits of autoregulation (LA). Hemodynamic and autoregulatory parameters were compared at three 24-hour intervals: baseline, before, and after intervention. Data were excluded if there were fewer than 6 hours of calculated autoregulatory parameters in any of the three epochs or greater than 4 hours between data availability and the intervention start or end.
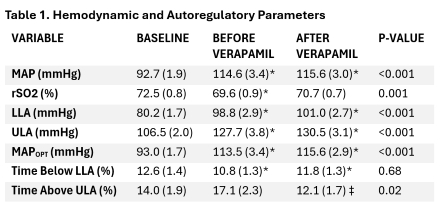
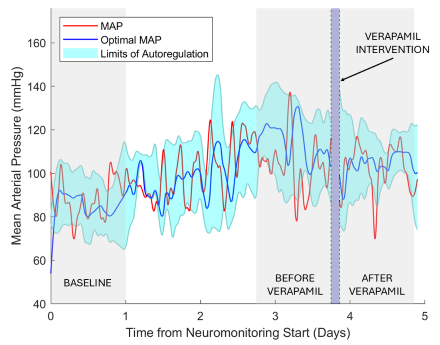
Results: The study included 27 interventions (mean verapamil dose 24 ± 10 mg, monitoring time 19.7 ± 3.5 hours per 24-hour period) across 15 patients (mean age 56 ± 11 years, 40% female, Hunt Hess 3.4 ± 0.9, modified Fisher 4 ± 0). From baseline (6.4 ± 3.8 days prior to intervention) to the time of intervention, there was a significant increase in actual MAP, MAPOPT, and LA (p<0.001), accompanied by a decrease in rSO2 (p=0.001, Table 1). Following intervention, the time spent above the upper limit of autoregulation decreased from 17.1 ± 2.3% to 12.1 ± 1.7% (p=0.02), while autoregulatory parameters and tissue oxygenation remained stable. Sensitivity analysis limited to the first intervention for each patient confirmed similar findings.
Conclusions: Our analysis demonstrated a decrease in tissue oxygenation and an increase in limits of autoregulation from baseline to the time when intervention was performed for vasospasm post-aSAH. IA verapamil administration was associated with a reduction in time spent above the upper limit of autoregulation, suggesting that pharmacologic spasmolysis for severe or refractory vasospasm may lead to improvement in autoregulatory physiology. Further exploratory analyses are ongoing.
More abstracts on this topic:
Bruce Samuel, Zhang Cenai, Liberman Ava, Merkler Alexander, Navi Babak, Chiang Gloria, Iadecola Costantino, Kamel Hooman, Murthy Santosh
Co-Expression Modules In The Periphreal Blood Transcriptome Following Subarachnoid Hemorrhage Associate With 90-Day OutcomeKnepp Bodie, Lenz Garreck, Hull Heather, Ko Nerissa, Jickling Glen, Choi H, Ander Bradley, Sharp Frank, Stamova Boryana
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.