Final ID: TP187
Automated Assessment of Intracerebral Hemorrhage Volumes using the VIOLA tool Performs Similarly to ABC/2 in Predictive Modelling
Methods: An ICH group was created by randomly sampling from the Registry for Neurological Endpoint Assessment among patients with Ischemic and Hemorrhagic Stroke (REINAH) database, which that includes completed hemorrhage characteristic assessments (location, laterality, volume calculated via ABC/2, and intraventricular hemorrhage (IVH) presence). Computed tomography (CT) images used for ABC/2 calculations were retrieved, and the previous trained VIOLA deep learning tool was deployed locally to calculate the volume of parenchymal and intraventricular hemorrhage. ICH volumes were compared using the Wilcoxon Signed Rank test, and separate multivariable logistic regression models to predict in-hospital mortality were fit, including patient demographics, comorbidities, clinical characteristics, and volume quartiles, and adjusted odds ratios are reported. Akaike information criteria (AIC) was used to compare separate ABC/2 and VIOLA models.
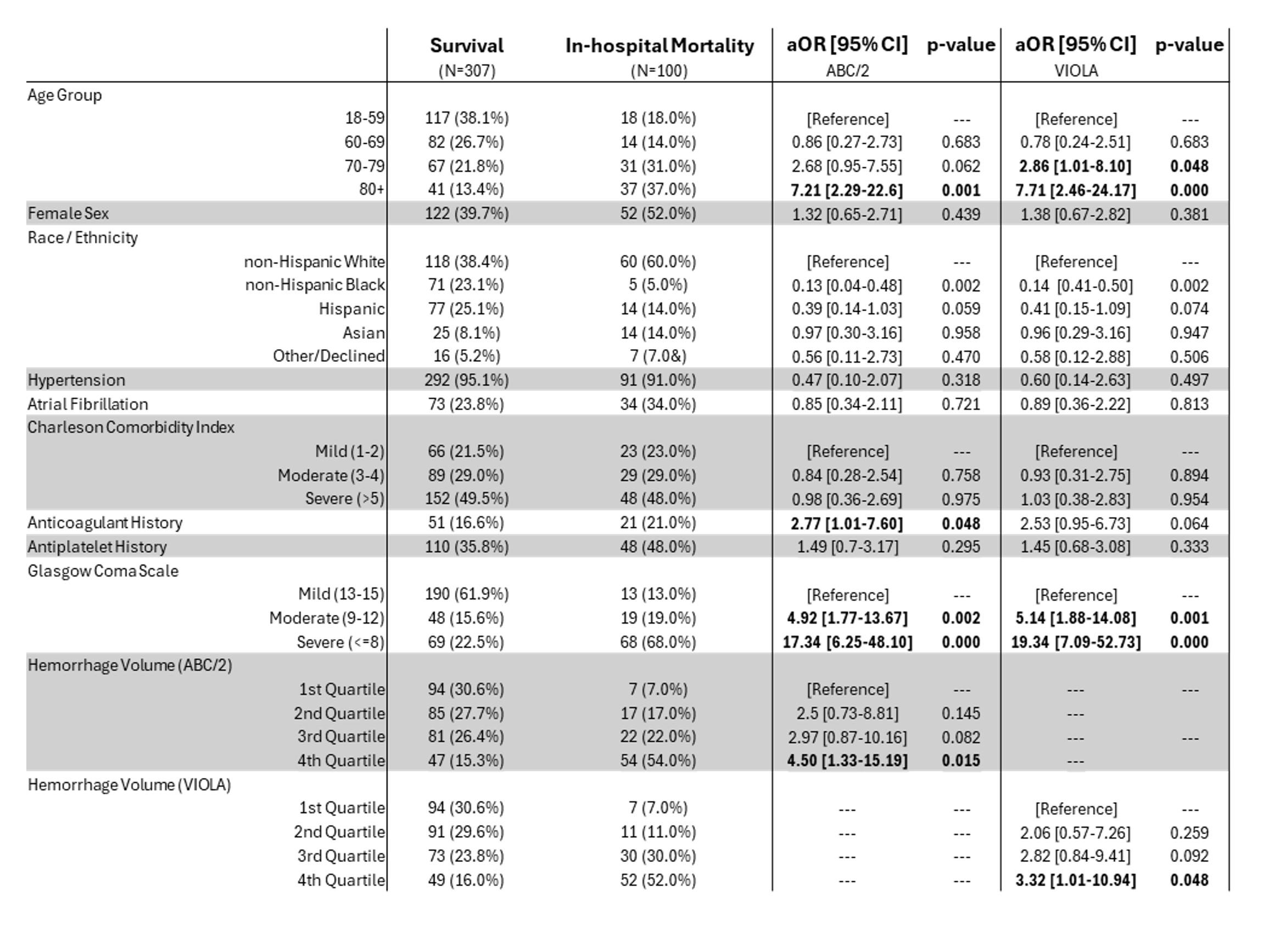
Results: A total of 407 patients were retrieved from RIENAH. Included patients had a median age of 68 [55-77], were 42.8% female, 43.7% White, 18.7% Black, 22.4% Hispanic, 9.6% Asian, and 5.7% Other/Declined. IVH was present in 48.4% of the cohort and 24.6% experienced in-hospital mortality. Hemorrhages assessed via VIOLA yielded a median of 23.70 [7.02-69.18] cm3, significantly higher than those determined by ABC/2 (14.33 [5.19-37.47] cm3,p<0.001), and more patients showed volumes over 30cm3 using VIOLA (78 (43.7%) vs 131 (32.2%)). In logistic regression modelling, patients with top-quartile hemorrhage volumes in either ABC/2 or VIOLA assessment had higher odds of in-hospital mortality (ABC/2 aOR: 3.32 [1.01-10.94]; VIOLA: 4.50 [1.33-15.19]). The VIOLA-based model showed similar AIC to the ABC/2 model, indicating roughly equivalent model fit (263.9 vs 261.9)
Discussion: Hemorrhage volume assessment using the VIOLA tool performed comparably than ABC/2 in prognostic modelling and provides a viable alternative to manual assessment.
More abstracts on this topic:
Nguyen Thuhien, Town James, Wahlster Sarah, Johnson Nicholas, Poilvert Nicolas, Lin Victor, Ukatu Hope, Matin Nassim, Davis Arielle, Taylor Breana, Thomas Penelope, Sharma Monisha
A Stepwise Approach to Identifying and Assessing the Content Validity of Patient-Reported Outcome (PRO) Measures for Use with Adults with Acute Heart FailureO'connor Meaghan, Loughlin Anita, Waldman Laura, Rucker Sloan, Vaghela Shailja, Kwon Namhee, Sikirica Vanja
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.