Final ID: WP122
Readmission to Acute Care from Inpatient Rehabilitation Among Patients with Acute Ischemic Stroke
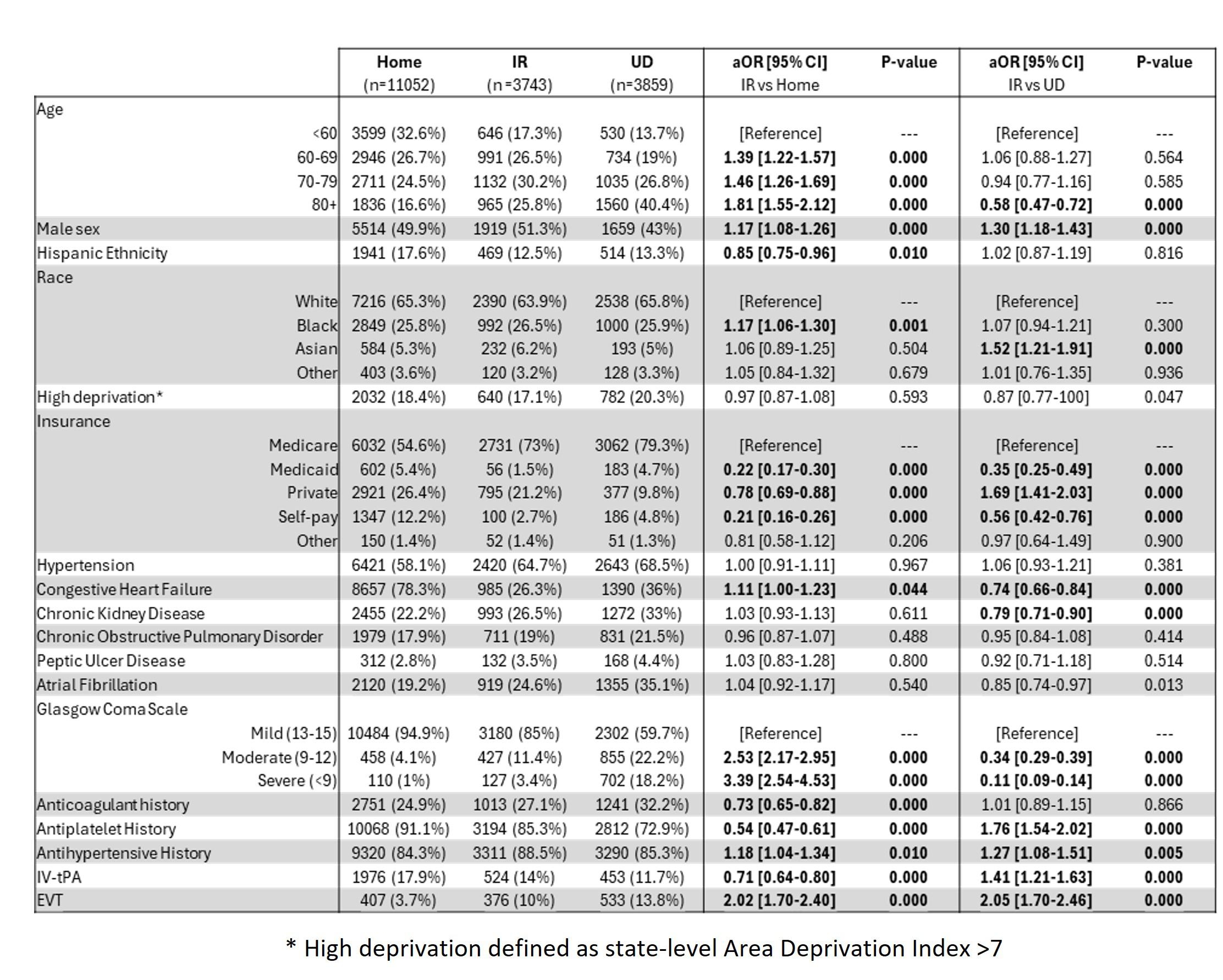
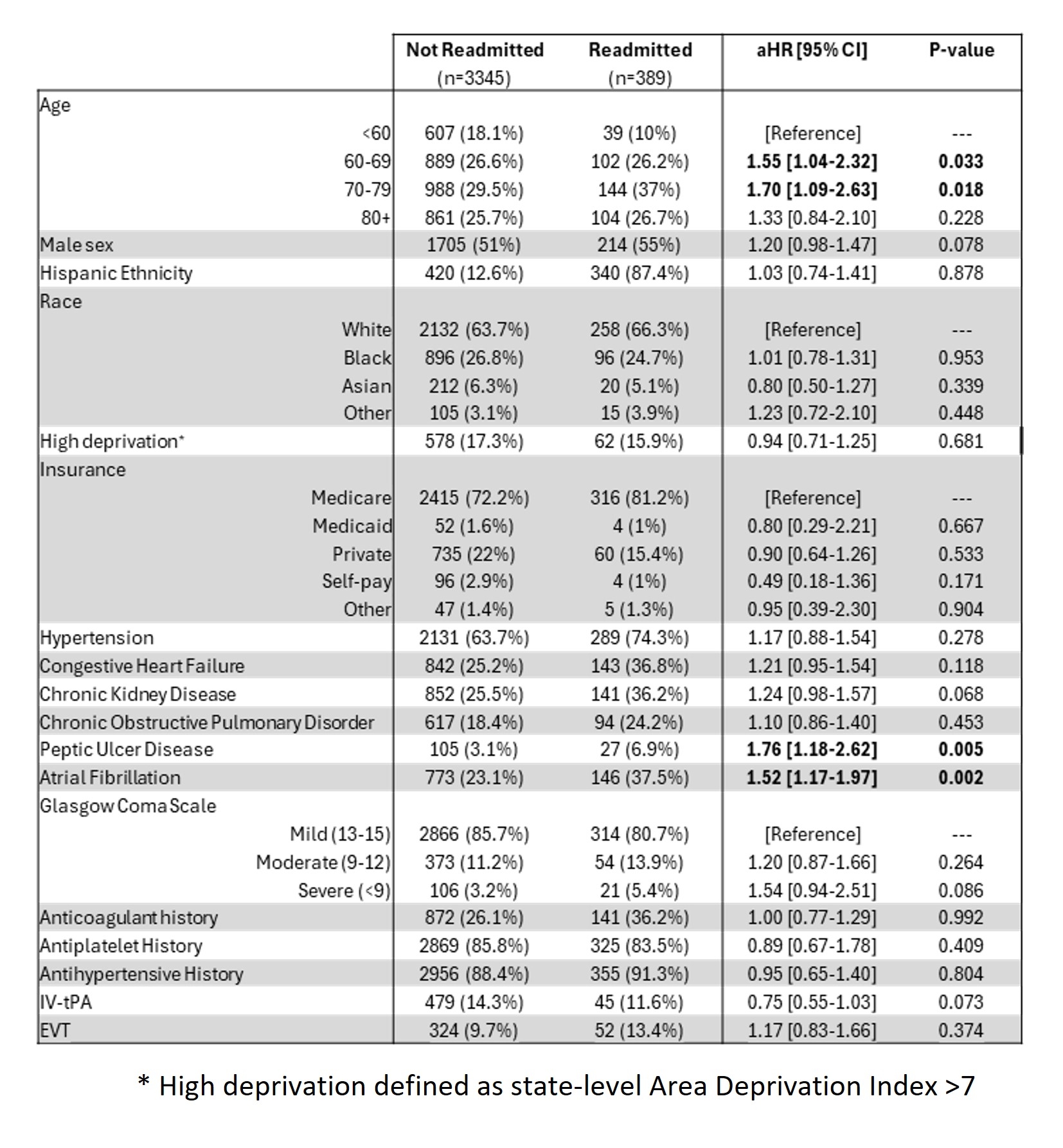
Methods: Data for adult (>18) AIS patients admitted from May 2016-May 2024 were retrieved from the Registry of Neurological Endpoint Assessment among Patients with Ischemic and Hemorrhagic Stroke (REINAH), including demographics, comorbidities, clinical scores, use of endovascular thrombectomy (EVT) and intravenous tissue plasminogen activator (IV-tPA), and discharge dispositions. Separate multivariable logistic regression models were fit to determine factors associated with discharge to IR vs. home (model 1) and IR vs. unfavorable discharge (UD; long-term acute care, skilled nursing facility, hospice, expired, other; model 2). Adjusted odds ratios (aOR) and 95% confidence intervals (CI) are reported. Cox proportional hazard models were fit to determine the hazard of 30-day RA for patients discharged to IR, with adjusted hazard ratios (aHR) and 95% CI reported.
Results: A total of 18,645 AIS patients were included, comprising 51.2% female and15.7% Hispanic patients with a racial distribution of 65.1% White, 26.0% Black, 5.4% Asian, and 3.5% Other. A total of 3,743 (20.0%) patients discharged to IR, 11,052 (59.3%) discharged home, and 3859 (20.7%) had UD. Of patients discharged to IR, 389 (10.4%) readmitted within 30 days. Across both IR discharge models, patients who were male (aORs: 1.17 [1.08-1.26]; 1.30 [1.18-1.43]), [FV2] had a history of antihypertensive use (1.18 [1.04-1.34]; 1.27 [1.08-1.51]), and received EVT (2.02 [1.70-2.40]; 2.05 [1.70-2.46]) were more likely to discharge to IR (vs. home or UD) (Figure 1). Consequently, patients who were self-pay (vs. Medicare, 1.17 [1.08-1.26]; 1.30 [1.18-1.43]) or on Medicaid (1.17 [1.08-1.26]; 1.30 [1.18-1.43]) had lower odds of discharge to IR (vs. home or UD). Among patients discharged to IR, those aged 60-69 years (vs. < 60) (aHR: 1.55 [1.04-2.32]), 70-79 years (1.70 [1.09-2.63]), with peptic ulcer disease (1.76 [1.18-2.62]) and atrial fibrillation (1.52 [1.17-1.97]) had higher odds of RA (Figure 2).
Discussion: Males and patients receiving EVT were more likely to discharge to IR, while those with peptic ulcer disease and atrial fibrillation who discharged to IR faced a greater risk of RA.
More abstracts on this topic:
Tezuka Yuji, Fujino Akiko, Ishii Mitsuru, Iguchi Moritake, Masunaga Nobutoyo, Esato Masahiro, Wada Hiromichi, Hasegawa Koji, Akao Masaharu, Oka Kouhei, Okamoto Keita, Yoshida Yusuke, Minami Kimihito, Ishigami Kenjiro, Doi Kosuke, Yoshizawa Takashi, Ide Yuya
A Multimodality Education Model Improves Healthcare Professionals' Competency in Managing Cardiovascular Risk Factors in Type 2 Diabetes: A Mixed-Methods StudyMadhusudhan Divya, Pressley Alyssa, El Sayed Nuha, Okeke Oge, Bradley Sarah, Blanco Caroline, Perla Esteban, Jennings Ruby, Picou Kylie, Mcweeny Patrick, Crabill Carrianne
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.