Final ID: TP303
Identifying Risk factors for Major Adverse Cardiovascular Events (MACE) in Patients with Migraine: A Logistic Regression Analysis of Demographics, Comorbidities, and Brain Imaging Findings
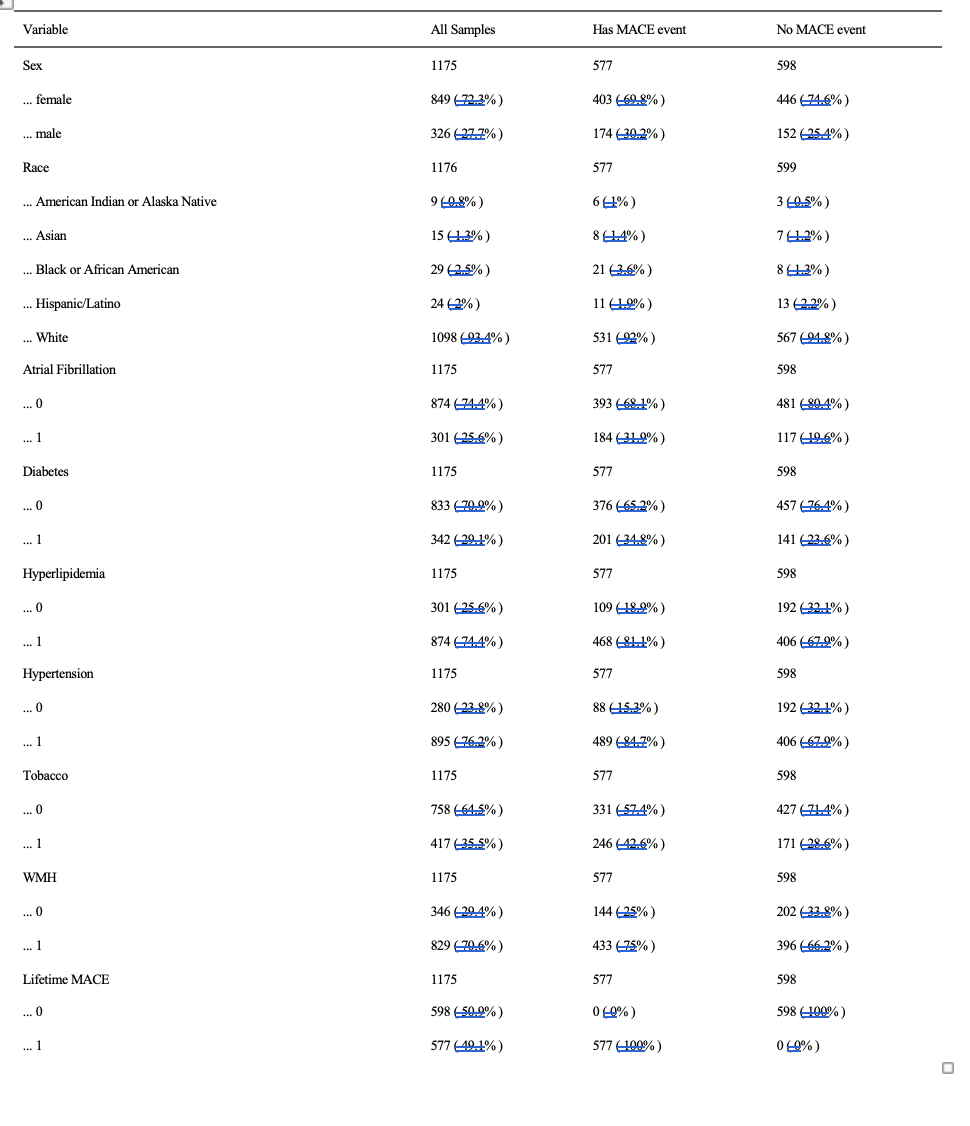
Methods: 60,454 patients, ages 18-89, with a ICD-9 or ICD-10 migraine diagnosis code in 2010 or later were identified from the Mayo Clinic electronic health record. Only patients who were seen for migraine in the Neurology Department were included. Patients with a migraine diagnosis who did not have MACE were included only if they had at least two visits at Mayo Clinic during five years. Only patients with sex and race information were included. The final cohort included 577 migraine patients with and 598 migraine patients without MACE. Presence of WMH was determined from radiology notes. Individuals without a brain MRI were assumed not to have WMH. A logistic regression model that included sex, race, known lifetime MACE risk factors (atrial fibrillation, diabetes, hypertension, hyperlipidemia, tobacco use) and WMH as independent variables to predict MACE outcome was fit.
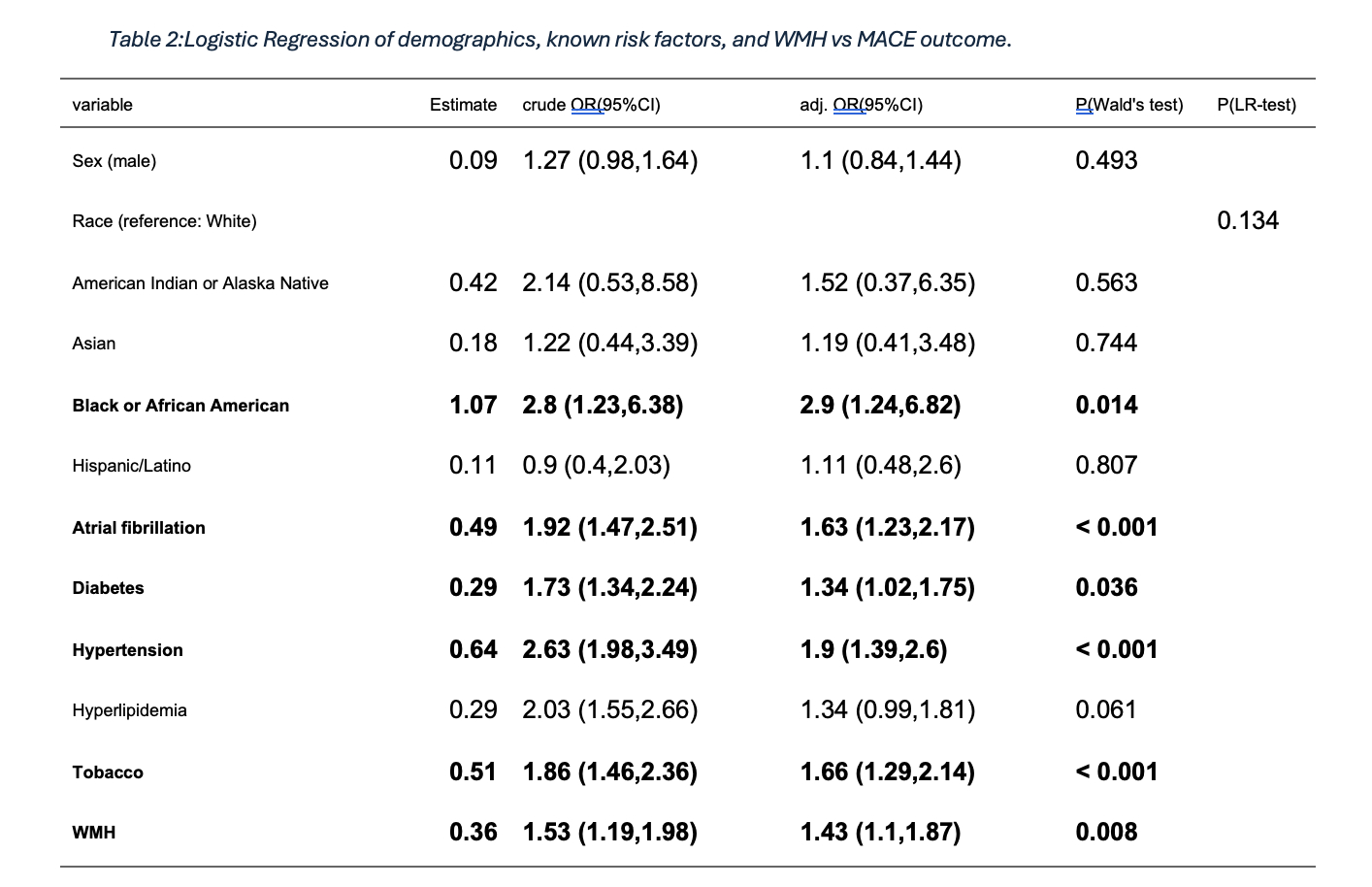
Results: Significant factors that increased the risk of MACE in individuals with migraine included being Black or African American (adjusted OR: 2.9, 95% CI: 1.24-6.82, p = 0.014), presence of atrial fibrillation (adj. OR: 1.63, 95% CI: 1.23-2.17, p < 0.001), diabetes (adj. OR: 1.34, 95% CI: 1.02-1.75, p = 0.036), hypertension (adj. OR: 1.9, 95% CI: 1.39-2.6, p < 0.001), tobacco use (adj. OR: 1.66, 95% CI: 1.29-2.14, p < 0.001), and the presence of WMH (adj. OR: 1.43, 95% CI: 1.1-1.87, p = 0.008). Hyperlipidemia showed a marginal association (adj. OR: 1.34, 95% CI: 0.99-1.81, p = 0.061), while other variables such as sex and other racial/ethnic groups did not significantly alter the risk of MACE outcome.
Discussion: Results indicate that African American race and presence of WMH in addition to common comorbidities independently increase the risk of MACE outcome.
More abstracts on this topic:
Wong Ka-ho, Krothapalli Neeharika, Littig Lauren, Champagne Alison, Majersik Jennifer, Reddy Vivek, De Havenon Adam
Calcitonin Gene-Related Peptide (CGRP) Inhibitor Use Is Associated With Increased Cardiovascular Event Risk in Patients with Migraine: A Nationwide StudyLusk Jay, Mac Grory Brian, Wilson Lauren, Moore Carlene, Yarnell Stephanie, Kalapura Cheryl, Choudhury Aparna, Schrag Matthew, Poli Sven, Li Fan
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.