Final ID: TP281
Prevalence of stroke in individuals with Migraine: A risk analysis accounting for comorbidities using participant information from the All of Us database
Method: Diagnoses of migraine, stroke and comorbidities were identified using ICD9 and ICD10 codes. A multivariable logistic regression analysis was performed to assess the association between migraine and risk of stroke adjusting for comorbidities including hypertension, atrial fibrillation, hyperlipidemia, diabetes, tobacco use, depression and demographics (age, sex at birth, race and ethnicity). To compare the prevalence of stroke between individuals with and without migraine, odds ratios using a 95% confidence interval (CI) were calculated.
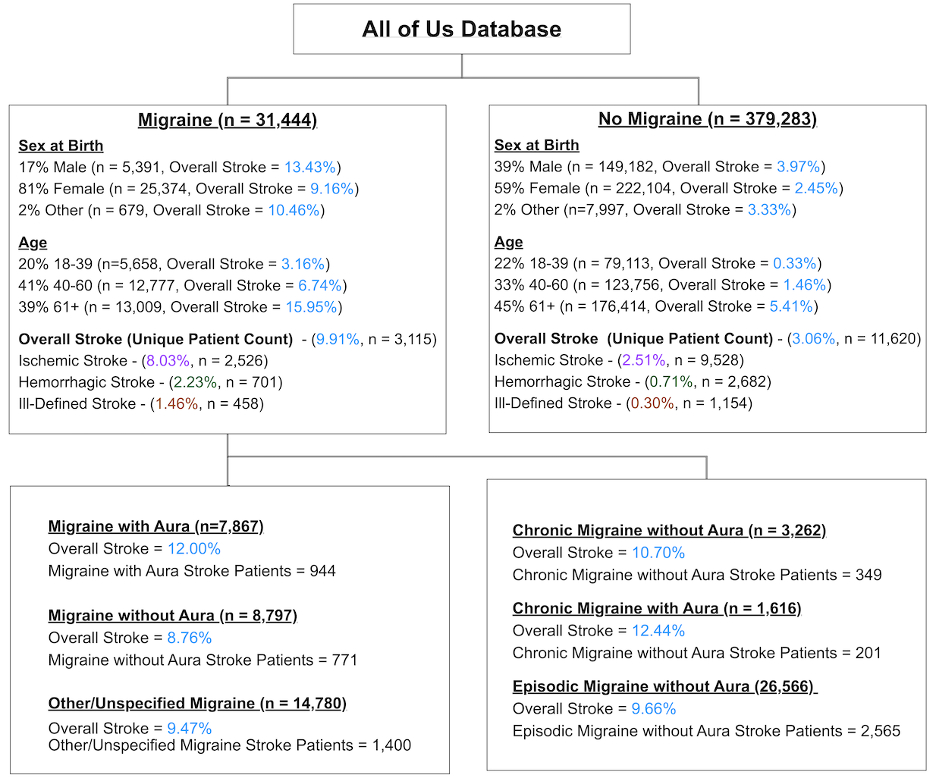
Results: Within the All of Us database, 31,444 individuals received a migraine diagnosis (female=25,374/81%, male=5,391/17%, other=679/2%; mean (std) age=54.9 (15.6)) and 379,283 did not have a migraine diagnosis (female=222,104/59%, male=149,182/39%, other=7,997/2%; mean (SD) age=55.9 (17.2)), see Figure 1 for detailed demographics.
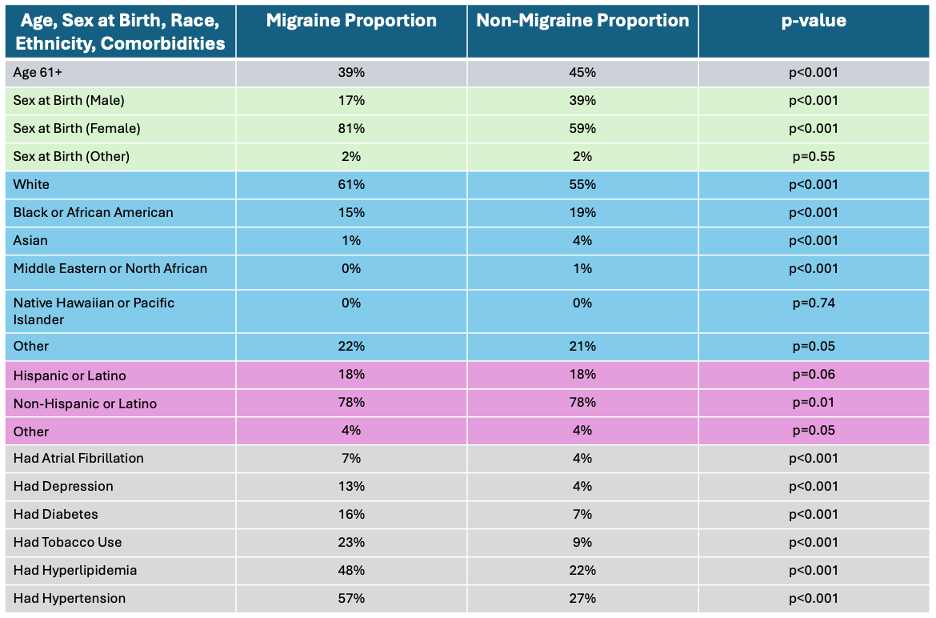
The migraine cohort had a greater proportion of women (81% vs 59%, p<0.001), a higher proportion of white individuals (61% vs. 55%, p<0.001) fewer African American individuals (15% vs. 19%, p<0.001) and a lower proportion of individuals who were 61 or older (39% vs 45%, p<0.001) compared to the non-migraine cohort.
Compared to the non-migraine cohort, individuals with migraine had significantly higher rates of comorbidities, including depression (13% vs. 4%, p<0.001), diabetes (16% vs. 7%), tobacco use (23% vs. 9%, p<0.001), hyperlipidemia (48% vs. 22%, p<0.001), hypertension (57% vs. 27%, p<0.001), and atrial fibrillation (7% vs. 4%, p<0.001).
A multivariate regression model adjusted for differences between cohort demographics and comorbidities found that individuals with migraine had 2.14 higher odds of overall stroke compared to the non-migraine cohort (OR 2.14, 95% CI [ 2.04, 2.24].
Discussion: After adjusting for cohort imbalances in demographics and comorbidities, individuals with migraine had a 2.14 times higher risk of stroke compared to those without a migraine diagnosis. Our analysis, using data from the All of Us database, confirms previous findings and suggests that while comorbidities are more prevalent in those with migraine, they do not fully account for the increased stroke risk.
More abstracts on this topic:
Lusk Jay, Mac Grory Brian, Wilson Lauren, Moore Carlene, Yarnell Stephanie, Kalapura Cheryl, Choudhury Aparna, Schrag Matthew, Poli Sven, Li Fan
A New Analytical Approach for Noninvasive Reconstruction of the Entire Left Ventricular Pressure Waveform in Myocardial Ischemia and InfarctionBilgi Coskun, Li Jiajun, Alavi Rashid, Dai Wangde, Matthews Ray, Kloner Robert, Pahlevan Niema
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.