Final ID: TP279
Predictive Modeling of Major Adverse Cardiovascular Events (MACE) in Patients with Migraine: Differential Performance for Ischemic and Hemorrhagic Stroke Outcomes
Abstract Body:
Introduction: Prior data suggest that migraine increases the risk of stroke. However, there is a lack of understanding whether specific migraine features like white matter hyperintensities (WMH) commonly found on brain magnetic resonance (MR) imaging in migraine patients and migraine medications might contribute to Major Adverse Cardiovascular Event (MACE) outcomes including ischemic and hemorrhagic stroke. We assess MACE risk estimation model stratified by event types using Mayo Clinic Electronic Health Record (EHR) data.
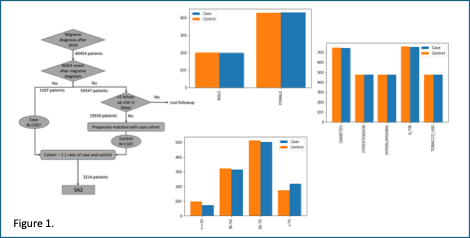
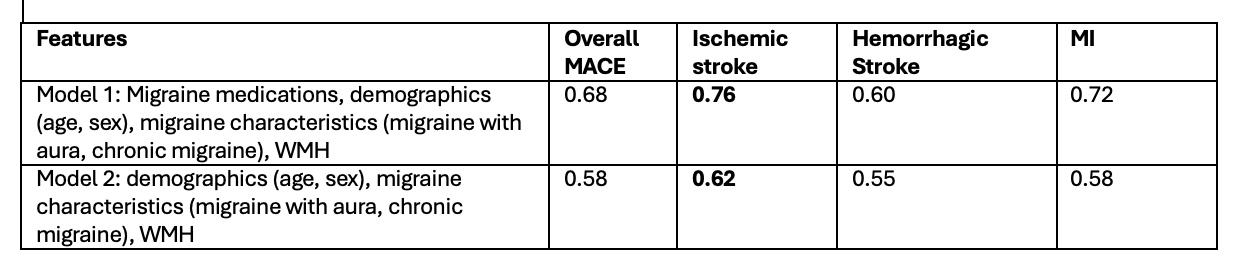
Methods: Case and control sets, based on MACE occurrence among migraine patients at Mayo Clinic Neurology Department, were propensity matched on age, sex, and MACE risk-factors (atrial fibrillation, diabetes, hyperlipidemia, hypertension, tobacco use) to capture migraine-specific predictors (Figure 1). Migraine medications were categorized into 9 classes; Triptans, Ditans, Gepants, Ergots, calcitonin gen-related peptide targeting medications (CGRPs), Beta-blockers, Topiramate, Tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors (SNRIs). Demographics (age and sex), migraine characteristics (chronic migraine, migraine with aura), and presence of WMH on MR imaging were curated. To model non-linear relationship between predictors, two comparative Random Forest (RF) models were evaluated for MACE prediction; i) Model-1: using demographics, migraine characteristics and WMH, ii) Model-2: medications, demographics, migraine characteristics and WMH (Table 1).
Results: Model-2 outperformed Model-1 indicating combined interaction between medications, WMH, and migraine characteristics for estimating MACE risk. Model-2 achieved AUC of 0.68 for overall MACE, but showed higher performance for ischemic stroke (AUC 0.76). We visualized the effects of input features on ischemic stroke risk for four individual patients using SHAP force plots (Figure 2). The model often considered use of betablockers, chronic migraine, and presence of WMH as factors for increasing ischemic stroke risk.
Discussion: Our experiments show that medications, migraine features, WMH and demographics are more effective estimators for ischemic risk stroke risk compared to overall MACE risk, indicating stronger predictive correlation between ischemic stroke and migraine related clinical features. Interestingly, the model inferred the clinical practice pattern of not prescribing Triptans (TRIPTAN=0) to the patients with high risk of stroke from the data itself.
Introduction: Prior data suggest that migraine increases the risk of stroke. However, there is a lack of understanding whether specific migraine features like white matter hyperintensities (WMH) commonly found on brain magnetic resonance (MR) imaging in migraine patients and migraine medications might contribute to Major Adverse Cardiovascular Event (MACE) outcomes including ischemic and hemorrhagic stroke. We assess MACE risk estimation model stratified by event types using Mayo Clinic Electronic Health Record (EHR) data.
Methods: Case and control sets, based on MACE occurrence among migraine patients at Mayo Clinic Neurology Department, were propensity matched on age, sex, and MACE risk-factors (atrial fibrillation, diabetes, hyperlipidemia, hypertension, tobacco use) to capture migraine-specific predictors (Figure 1). Migraine medications were categorized into 9 classes; Triptans, Ditans, Gepants, Ergots, calcitonin gen-related peptide targeting medications (CGRPs), Beta-blockers, Topiramate, Tricyclic antidepressants, serotonin-norepinephrine reuptake inhibitors (SNRIs). Demographics (age and sex), migraine characteristics (chronic migraine, migraine with aura), and presence of WMH on MR imaging were curated. To model non-linear relationship between predictors, two comparative Random Forest (RF) models were evaluated for MACE prediction; i) Model-1: using demographics, migraine characteristics and WMH, ii) Model-2: medications, demographics, migraine characteristics and WMH (Table 1).
Results: Model-2 outperformed Model-1 indicating combined interaction between medications, WMH, and migraine characteristics for estimating MACE risk. Model-2 achieved AUC of 0.68 for overall MACE, but showed higher performance for ischemic stroke (AUC 0.76). We visualized the effects of input features on ischemic stroke risk for four individual patients using SHAP force plots (Figure 2). The model often considered use of betablockers, chronic migraine, and presence of WMH as factors for increasing ischemic stroke risk.
Discussion: Our experiments show that medications, migraine features, WMH and demographics are more effective estimators for ischemic risk stroke risk compared to overall MACE risk, indicating stronger predictive correlation between ischemic stroke and migraine related clinical features. Interestingly, the model inferred the clinical practice pattern of not prescribing Triptans (TRIPTAN=0) to the patients with high risk of stroke from the data itself.
More abstracts on this topic:
A Machine Learning Approach to Predict Percutaneous Coronary Intervention in Patients with Critical Illness and Signs of Myocardial Injury
Mueller Joshua, Stepanova Daria, Chidambaram Vignesh, Nakarmi Ukash, Al'aref Subhi
Anatomic Physiological Scoring is a Comparable Predictor of Adult Congenital Operative Morbidity and MortalityLa Brenda, Taylor-fishwick Jon, Macbeth Morgan, Soohoo Megan
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.
Rate this abstract
(Maximum characters: 500)