Final ID: WP99
Target door-to-needle time in acute stroke treatment via telemedicine versus in-person evaluation in a rural setting of the Midwest: preliminary data analysis
Telemedicine enables stroke specialists to treat patients with suspected acute stroke in facilities lacking in-person coverage. Studies have compared telemedicine in rural settings to in-person evaluation in urban areas, introducing biases of different infrastructure capabilities and ancillary staff. In this study, the authors provide a comparison of door-to-needle time (DTN) in the administration of thrombolytics in a rural stroke network, where the acute stroke care is provided by the same stroke specialists both in-person and via telemedicine.
Methods
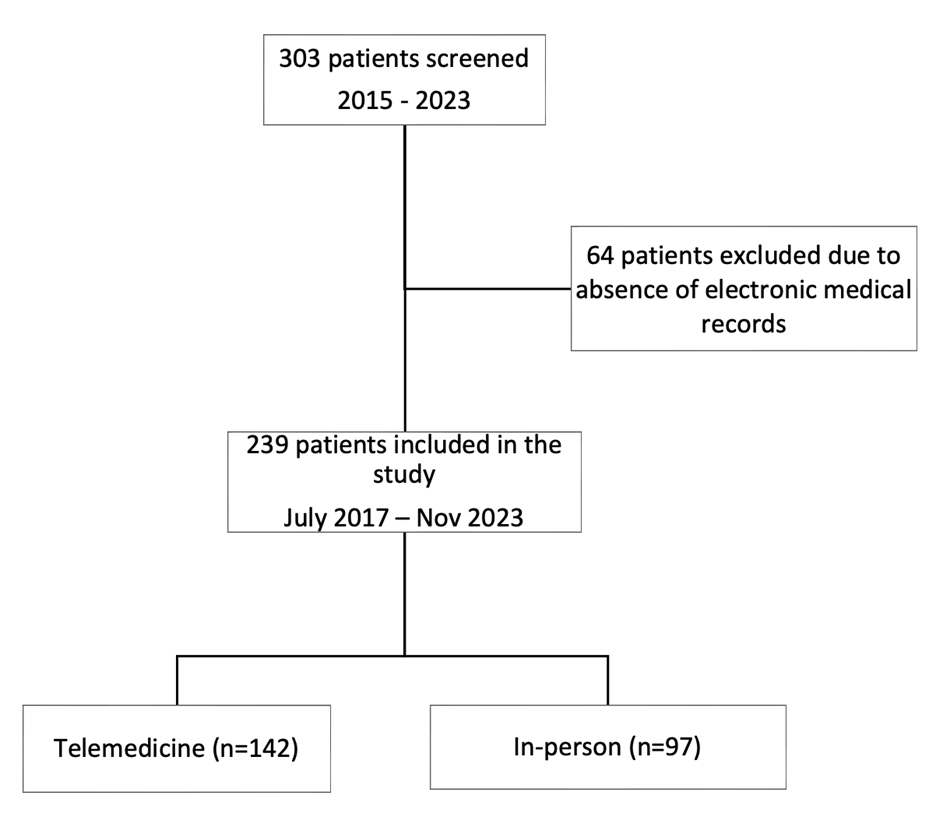
This is a retrospective study analyzing DTN in patients treated with thrombolytics at a rural stroke network over a five-year period. For each patient, demographics, medical history, clinical presentation, modality of evaluation, facilitator of telemedicine, and DTN were reviewed. Thrombolytic complications, mortality, and mRS at one month were noted.
Results
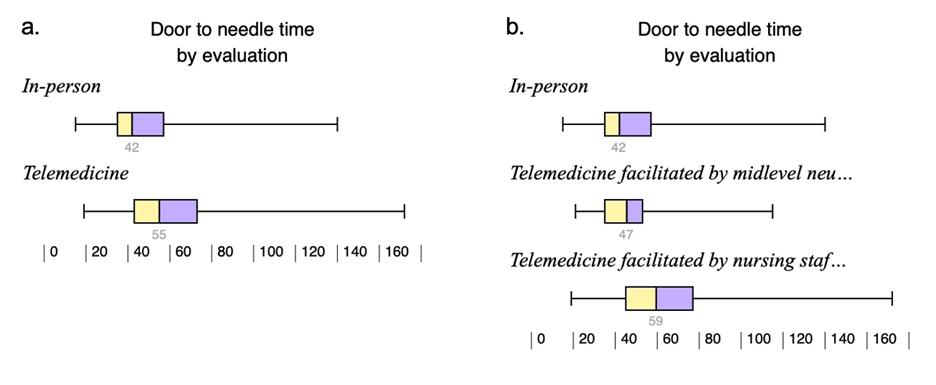
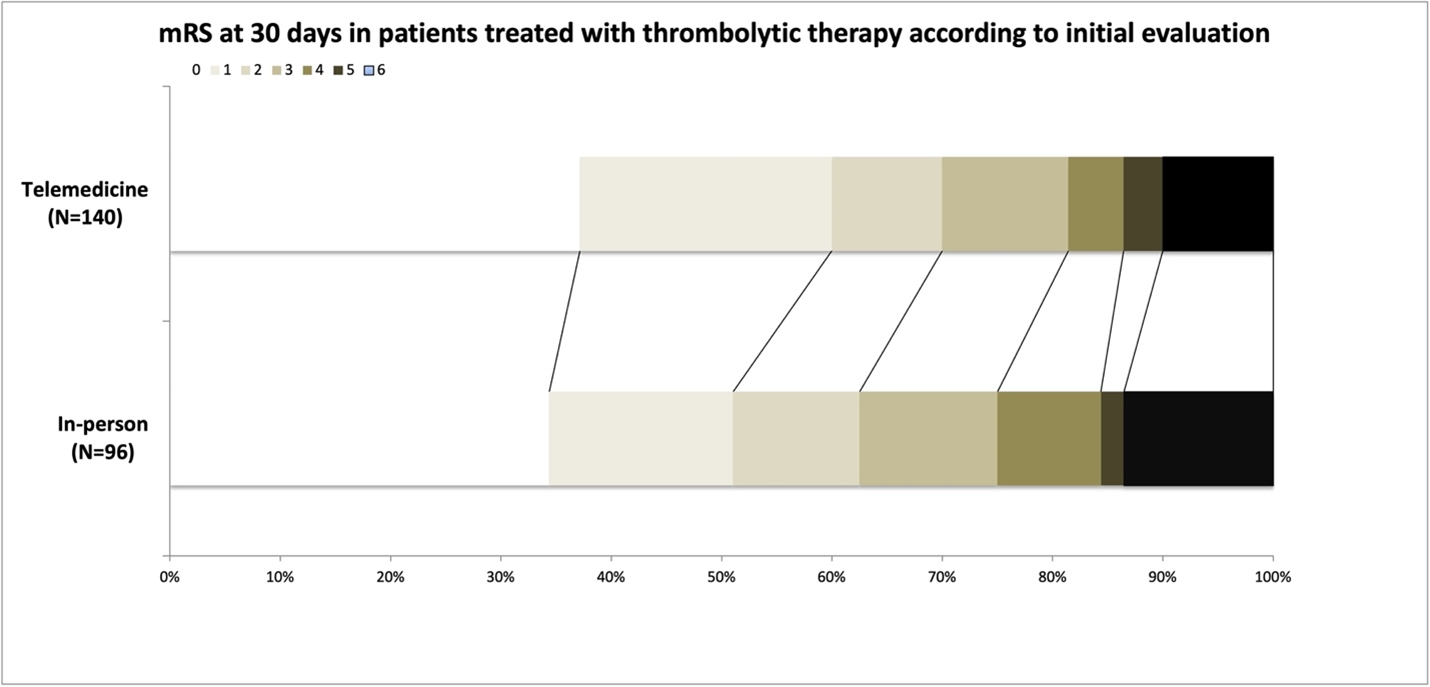
Out of 239 patients treated with thrombolytics, 142 were evaluated by telemedicine, and 97 in-person. In the telemedicine group, 108 evaluations were facilitated by nursing staff, while 34 were facilitated by midlevel neurology providers (MNP). The in-person group was associated with a faster median DTN, in minutes, (42(35-54) vs. 55(43-73), p<0.01) and higher rate of DTN≤60 minutes (76% vs. 60%, p=0.01). In a logistic regression model, after correcting for NIHSS, GCS, SBP, time of evaluation, and presence of family at bedside, in-person evaluation remained associated with better DTN (OR:2.02, CI:1.06-3.81, p=0.03). There was no difference between the two groups in safety and short-term outcome. The presence of MNP as telemedicine facilitator improved both DTN (47(35-53) vs. 42(35-54)) and DTN≤60 minutes (85% vs. 76%) compared to in-person evaluation (p>0.05 for both).
Conclusions
In our population, in-person evaluation provided faster DTN compared to telemedicine. This trend reversed when a midlevel provider facilitated telemedicine. The faster DTN did not translate into increased safety or better short-term outcome. Larger studies are needed to understand the underlying causes of these differences in stroke metric.
More abstracts on this topic:
Elfil Mohamed, Malik Amer, Al-mufti Fawaz, Abbas Abdallah, Fountain Hayes, Abdul-hamid Ebrahem, Aladawi Mohammad, Najdawi Zaid, Elmashad Ahmed, Ghaith Hazem, Dawod Giana
Endovascular Treatment Versus Best Medical Therapy for Acute Ischemic Stroke Due to Medium or Distal Vessel Occlusions: A Meta-Analysis of Randomized Controlled TrialsObi Ogechukwu, Nweze Uchenna, Unegbe Chinenye, Asonye Patricia, Lajczak Pawel
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.