Final ID: TP91
Comparison of telemedicine-administered thrombolytic therapy for acute ischemic stroke by neurology subspecialty: preliminary data analysis
To determine if any difference exists in safety and outcomes of patients treated with thrombolytic therapy via telemedicine, based on the subspeciality of the treating neurologist.
Methods
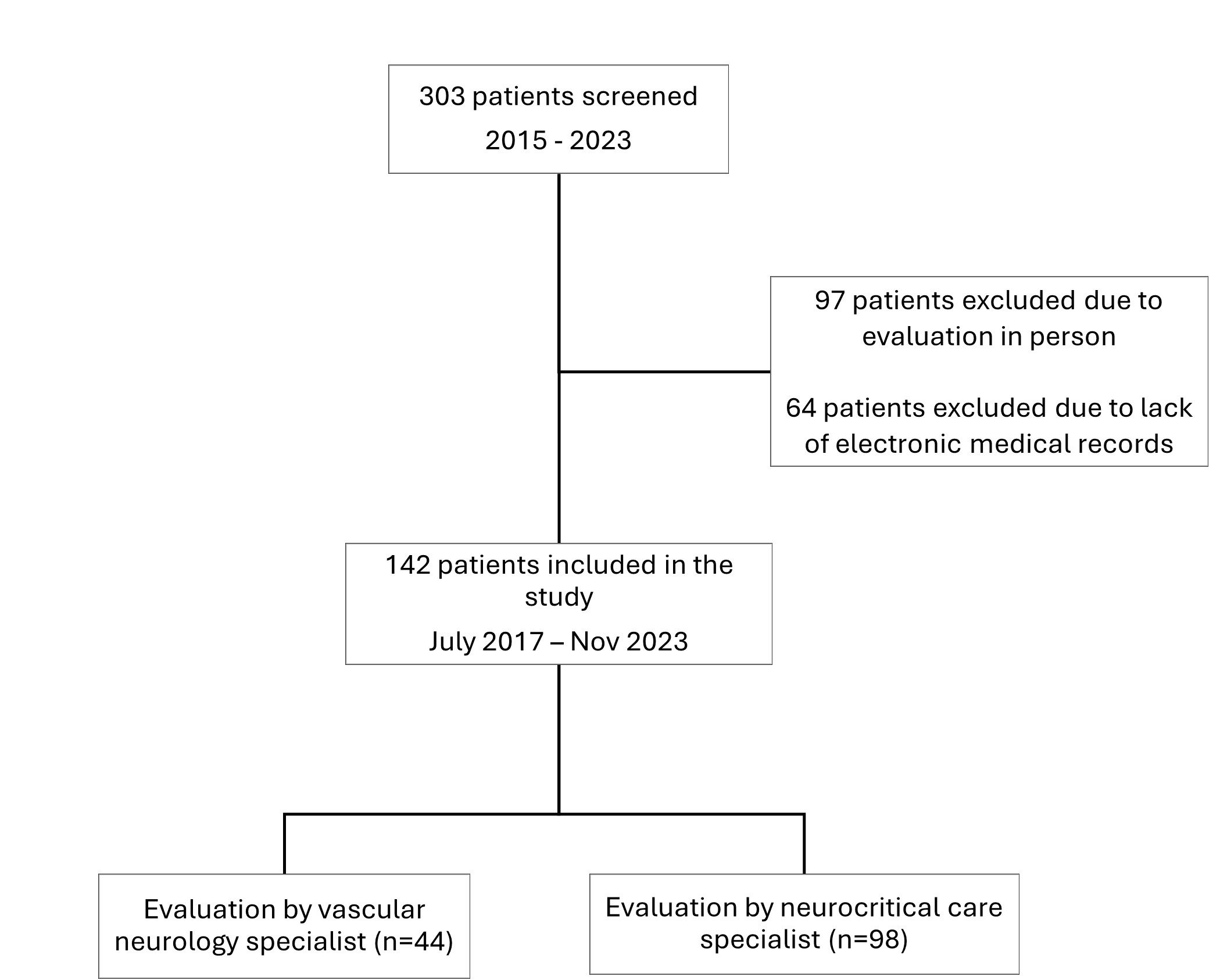
We performed a retrospective cross-sectional study using data from our local stroke registry of patients evaluated via telemedicine and treated with thrombolytic therapy at our rural stroke network over five years. The cohort was divided into two groups based on the subspecialty of the treating neurologist: vascular neurology (VN) and neurocritical care (NCC). Demographics, clinical characteristics, stroke metrics, thrombolytic complications, and final diagnosis were reviewed. In-hospital mortality and mRS at 30 days were noted. Primary outcome was symptomatic intracerebral hemorrhage (sICH); secondary outcome was mRS 0-1 at 30 days.
Results
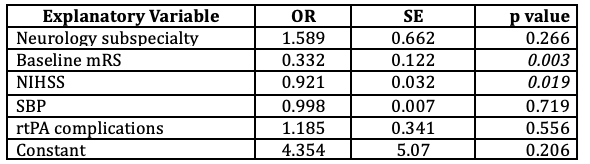
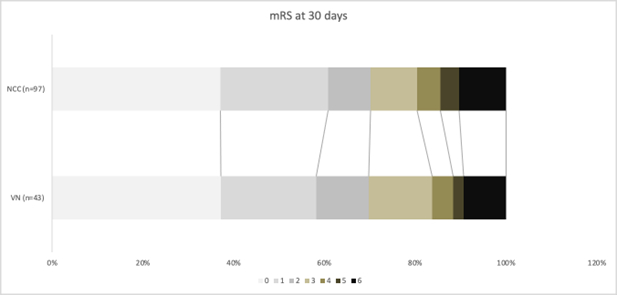
Among 142 patients who received thrombolytic therapy via telemedicine, 44 (31%) were evaluated by a VN specialist, whereas 98 (69%) by an NCC specialist. There was no difference in baseline clinical characteristics between the VN and NCC groups. The stroke metrics, including door-to-needle time within 60 minutes (55% vs. 62%), and final diagnosis of ischemic stroke (64% vs. 60%), were similar between the two groups (p>0.5 for all). Compared to NCC group, VN group had a higher trend of sICH (7% vs. 1%, p=0.05). However, in a logistic regression analysis, after correcting for NIHSS, SBP, door-to-needle time, and baseline use of antiplatelet therapy, the type of neurology subspecialty was not independently associated with development of sICH (OR 0.141, SE 0.188, p=0.141). The rate of in-hospital mortality was also similar between VN and NCC (7% vs. 5%, p=0.8). In a model that accounted for stroke severity, no association was established between the type of neurology subspecialty and mRS at 30 days (OR 1.589, SE 0.662, p=0.266)
Conclusions
In our population, safety and outcome of thrombolytic therapy via telemedicine were not influenced by the subspecialty of treating neurologist. Our study supports the continued use and expansion of telemedicine in acute stroke care, leveraging the expertise of both vascular neurologists and neurocritical care specialists to improve accessibility and outcomes for patients in rural and underserved areas.
More abstracts on this topic:
Kang Junghee, Moser Debra, Cha Geunyeong, Lin Chin-yen, Wu Jia-rong, Okoli Chizimuzo, Latimer Abigail, Lennie Terry, Biddle Martha, Chung Misook
Assessing the Impact of Remote Consultation Strategies on Optimizing Guideline-Directed Medical Therapy in Heart Failure Patients: A Meta-AnalysisAlzubi Alhasan Saleh, Mohamed Mohamed Barakat Mohamed, Elfaituri Ahmed, Elhadi Muhammed, S. Beshr Mohammed, Abdelwahed Abdelrahman Farag, Abuajamieh Maram, Elmesherghi Abdulmoez Fauzi, Ekreer Moad, Alawi Zahra Sayed Jalal, Azlitni Muhab, El Awami Mostafa
Readers' Comments
We encourage you to enter the discussion by posting your comments and questions below.
Presenters will be notified of your post so that they can respond as appropriate.
This discussion platform is provided to foster engagement, and simulate conversation and knowledge sharing.
You have to be authorized to post a comment. Please, Login or Signup.