Final ID: TH159
Rising Mortality from Chronic Kidney Disease in the United States: A 22-Year National Analysis of Trends and Disparities (1999–2020)
Abstract Body: Introduction: Chronic kidney disease (CKD) affects an estimated 37 million adults in the United States and contributes substantially to cardiovascular mortality. While clinical awareness and management strategies have improved, national trends in CKD-related mortality and disparities across sex, race, and geography remain insufficiently characterized.
Hypothesis: We hypothesized that CKD-related mortality has increased over the past two decades and exhibits significant disparities across sex, race, and geographic location in the United States.
Methods: We analyzed 512,421 mortality records from the CDC WONDER database from 1999 to 2020 for individuals aged >35 years with CKD (ICD-10: N18) listed as the underlying cause of death. Age-adjusted mortality rates (AAMRs) per 100,000 were calculated. Temporal trends and annual percent change (APC) were assessed using Joinpoint regression.
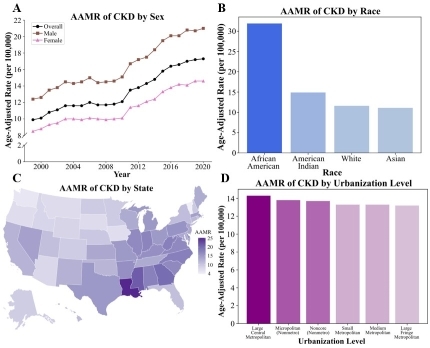
Results: From 1999 to 2020, the CKD-related AAMR significantly increased from 9.9 (95% CI, 9.7–10.0) to 17.3 (95% CI, 17.1–17.5), with an APC of 2.8% (p<0.001). Males exhibited a higher cumulative AAMR than females (16.9 [95% CI, 16.8–16.9] vs. 11.5 [95% CI, 11.4–11.5]). Among racial groups, African Americans had the highest AAMR (31.9 [95% CI, 31.7–32.1]), followed by American Indians (14.9 [95% CI, 14.4–15.4]), Whites (11.6 [95% CI, 11.6–11.7]), and Asians (11.1 [95% CI, 10.9–11.3]). Large urban metropolitan areas showed slightly higher AAMRs than rural noncore areas (14.3 [95% CI, 14.2–14.3] vs. 13.7 [95% CI, 13.5–13.8]). Regionally, the South had the highest AAMR (15.4 [95% CI, 15.3–15.4]), followed by the Midwest (14.2 [95% CI, 14.1–14.3]), Northeast (13.0 [95% CI, 12.9–13.1]), and West (10.4 [95% CI, 10.4–10.5]).
Conclusions: Mortality from CKD has risen significantly over the past two decades, with disproportionate impacts on males, African Americans, and residents of large metropolitan areas and the Southern United States. To combat this burden, public health interventions may include earlier screening for endothelial dysfunction, improved access to nephrology care, and community-based efforts to address the structural drivers of CKD progression.
Hypothesis: We hypothesized that CKD-related mortality has increased over the past two decades and exhibits significant disparities across sex, race, and geographic location in the United States.
Methods: We analyzed 512,421 mortality records from the CDC WONDER database from 1999 to 2020 for individuals aged >35 years with CKD (ICD-10: N18) listed as the underlying cause of death. Age-adjusted mortality rates (AAMRs) per 100,000 were calculated. Temporal trends and annual percent change (APC) were assessed using Joinpoint regression.
Results: From 1999 to 2020, the CKD-related AAMR significantly increased from 9.9 (95% CI, 9.7–10.0) to 17.3 (95% CI, 17.1–17.5), with an APC of 2.8% (p<0.001). Males exhibited a higher cumulative AAMR than females (16.9 [95% CI, 16.8–16.9] vs. 11.5 [95% CI, 11.4–11.5]). Among racial groups, African Americans had the highest AAMR (31.9 [95% CI, 31.7–32.1]), followed by American Indians (14.9 [95% CI, 14.4–15.4]), Whites (11.6 [95% CI, 11.6–11.7]), and Asians (11.1 [95% CI, 10.9–11.3]). Large urban metropolitan areas showed slightly higher AAMRs than rural noncore areas (14.3 [95% CI, 14.2–14.3] vs. 13.7 [95% CI, 13.5–13.8]). Regionally, the South had the highest AAMR (15.4 [95% CI, 15.3–15.4]), followed by the Midwest (14.2 [95% CI, 14.1–14.3]), Northeast (13.0 [95% CI, 12.9–13.1]), and West (10.4 [95% CI, 10.4–10.5]).
Conclusions: Mortality from CKD has risen significantly over the past two decades, with disproportionate impacts on males, African Americans, and residents of large metropolitan areas and the Southern United States. To combat this burden, public health interventions may include earlier screening for endothelial dysfunction, improved access to nephrology care, and community-based efforts to address the structural drivers of CKD progression.
More abstracts on this topic:
Adoptive Transfer of Lupus Patient PBMCs Promotes Salt-Sensitive Hypertension and Kidney Injury in Immunodeficient Mice
Saleem Mohammad, Ormseth Michelle, Kirabo Annet, Ahmad Taseer, Haynes Alexandria, Albritton Claude, Arshad Suha, Kulapatana Phicharmon, Posey Olivia, Major Amy, Stein Charles
A Community-Based Intervention to Improve Cardiovascular Health Understanding in the Dallas-Fort Worth South Asian CommunityDeo Parminder, Rohatgi Anand, Sharma Parul, Sathyamoorthy Mohanakrishnan