Final ID: TH188
Comparative Analysis of Hypertension-Associated Cancer Mortality Trends: Urinary Tract Versus All Cancers Using CDC WONDER and ARIMA Modeling (1999–2030)
Abstract Body: Introduction: Dose-dependent hypertension associations with urinary tract cancers have been demonstrated in cohort-based studies by Teleka S. et al. (2018, 2020, 2021). Building on these findings, this study aims to explore the impact of hypertension on mortality trends specifically for urinary tract cancers compared to all cancers, using population-based data from the CDC WONDER database.
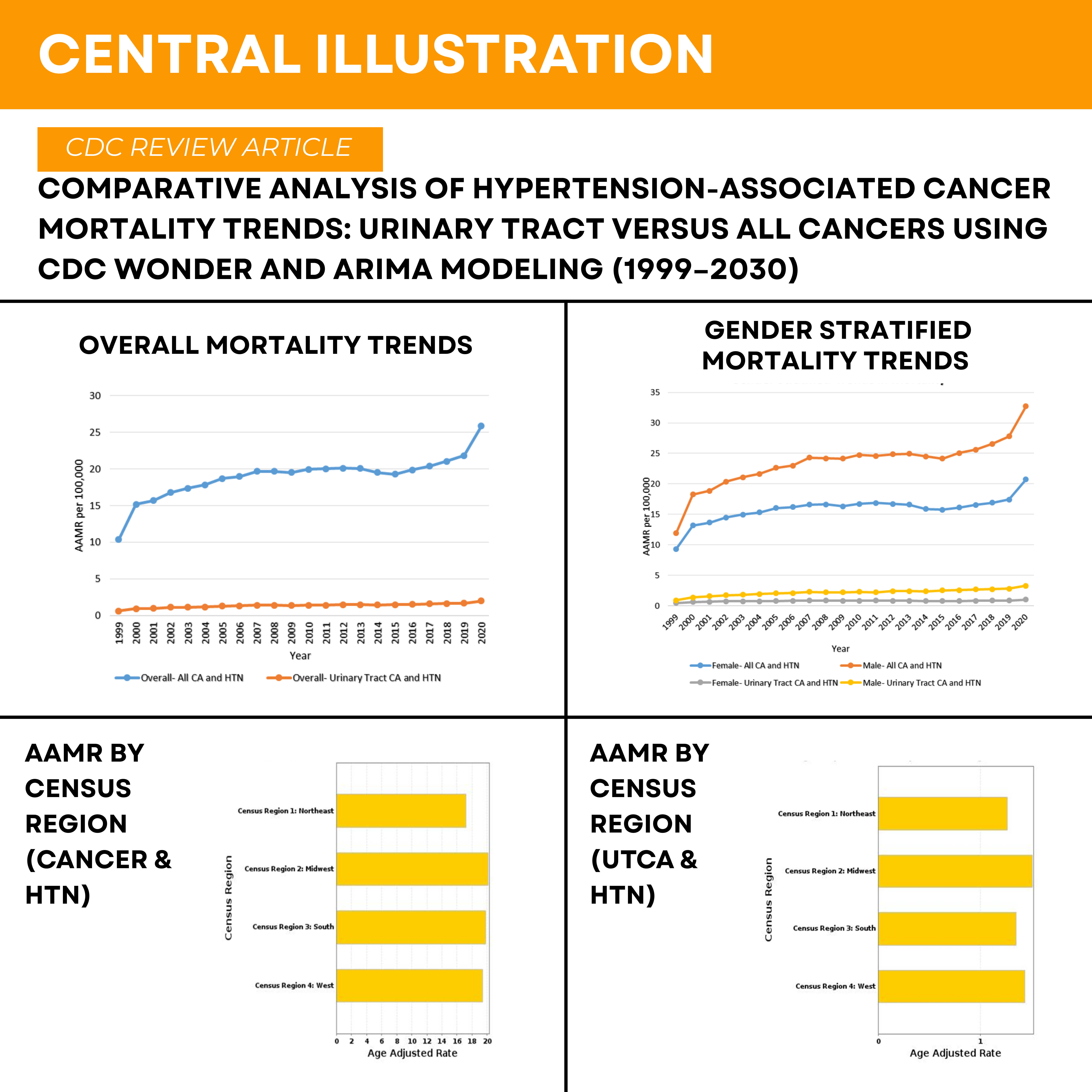
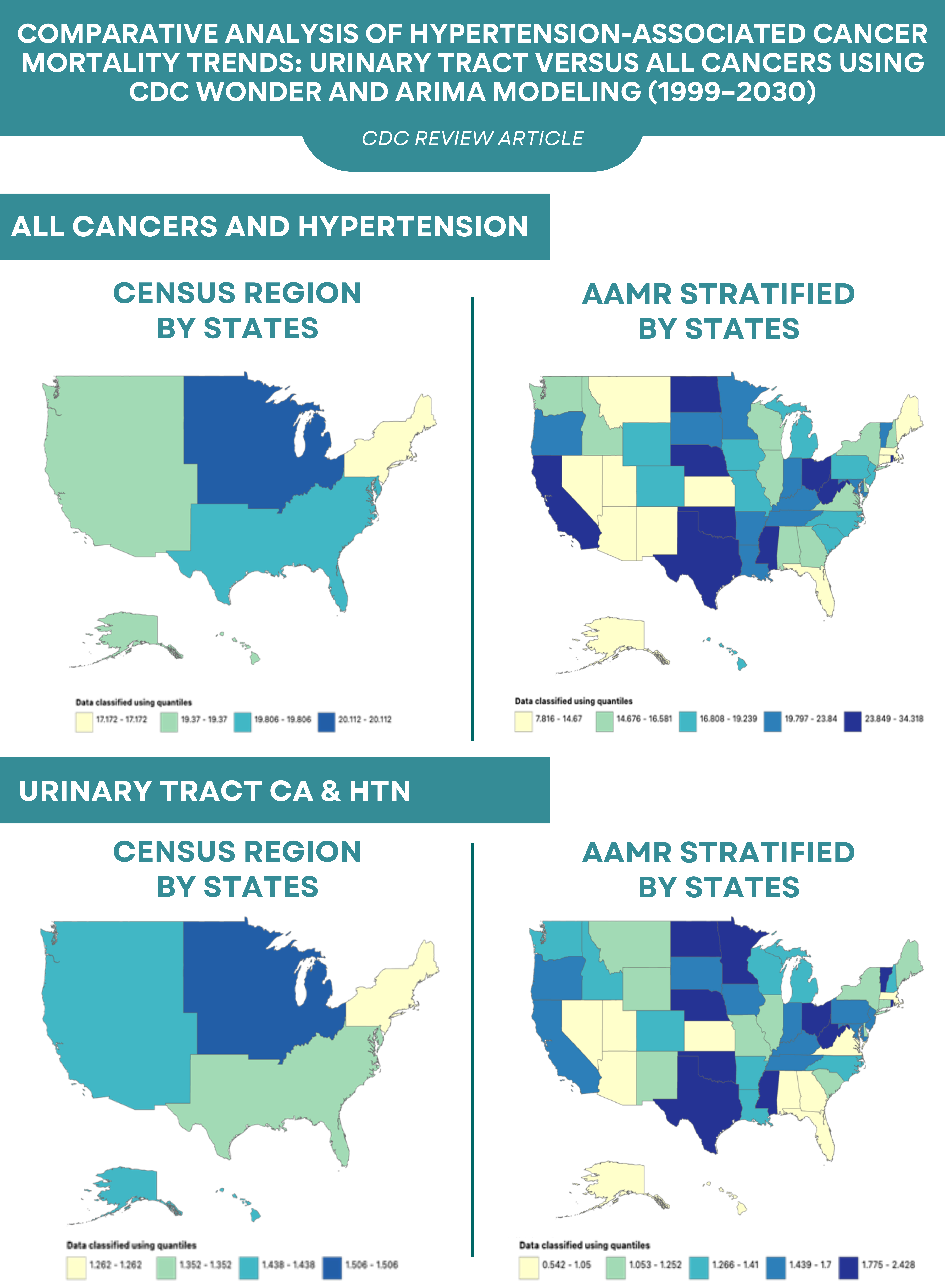
Methodology: CDC WONDER data for Urinary Tract cancer (C64-C68, D30) deaths with underlying hypertension (I10-I15) were analyzed for Cohort 1, and for Cohort 2, all cancer (C00-D48) deaths with hypertension as a contributing cause. Data were stratified by gender, race, origin, region, and urbanization. Age-adjusted mortality rates (AAMRs) and annual percentage changes (APCs) were calculated using Joinpoint regression (p<0.05). The ARIMA (Autoregressive Integrated Moving Average) model with Box-Cox transformation, along with ADS and KPSS-based stationary testing, was applied.
Results: The mean AAPC from 1999 to 2020 for Cohort 1 was 5.15 (95% CI: 0.03 to 6.28; P < 0.0001), compared to 3.96 (95% CI: 3.16 to 4.78; P < 0.0001) for Cohort 2. Between 2018 and 2020, Cohort 1 demonstrated a significant upward trend (APC: 11.09; 95% CI: 5.38–17.11), with ARIMA forecasting a decline to 2.57 by 2030 (95% CI: 2.03–3.09; MAPE: 5.31%). Cohort 2 showed a steeper increase (APC: 12.29; 95% CI: 7.78–17.00), with projections indicating a continued rise to 31.80 by 2030 (95% CI: 25.42–37.65; MAPE: 6.13%). In Cohort 1, the mean AAPC was higher in males (5.90; 95% CI: 4.25–7.56) than in females (3.60; 95% CI: 2.13–5.09). Comparable trends were observed in Cohort 2, with AAPCs of 4.37 (95% CI: 3.62–5.12) in males and 3.43 (95% CI: 2.48–4.39) in females. In the South (Census Region 3), Cohort 1 demonstrated a substantially higher mean APC of 6.59 (95% CI: 4.56–8.67) compared to 3.19 (95% CI: 2.28–4.12) in Cohort 2. Among Hispanics, Cohort 1 had a mean APC of 6.57 (95% CI: 1.12–12.31), compared to 4.06 (95% CI: 2.69–5.45) in Cohort 2. Among White individuals, Cohort 1 showed a higher APC of 5.49 (95% CI: 4.39–6.60) versus 4.30 (95% CI: 3.33–5.27) in Cohort 2.
Conclusion: Cohort 1 demonstrated higher mortality trends across multiple subgroups, indicating a disproportionate burden of mortality in this high-risk group. However, ARIMA projections suggest that while Cohort 1's trend declines by 2030, Cohort 2 will continue to rise, potentially surpassing Cohort 1.
Methodology: CDC WONDER data for Urinary Tract cancer (C64-C68, D30) deaths with underlying hypertension (I10-I15) were analyzed for Cohort 1, and for Cohort 2, all cancer (C00-D48) deaths with hypertension as a contributing cause. Data were stratified by gender, race, origin, region, and urbanization. Age-adjusted mortality rates (AAMRs) and annual percentage changes (APCs) were calculated using Joinpoint regression (p<0.05). The ARIMA (Autoregressive Integrated Moving Average) model with Box-Cox transformation, along with ADS and KPSS-based stationary testing, was applied.
Results: The mean AAPC from 1999 to 2020 for Cohort 1 was 5.15 (95% CI: 0.03 to 6.28; P < 0.0001), compared to 3.96 (95% CI: 3.16 to 4.78; P < 0.0001) for Cohort 2. Between 2018 and 2020, Cohort 1 demonstrated a significant upward trend (APC: 11.09; 95% CI: 5.38–17.11), with ARIMA forecasting a decline to 2.57 by 2030 (95% CI: 2.03–3.09; MAPE: 5.31%). Cohort 2 showed a steeper increase (APC: 12.29; 95% CI: 7.78–17.00), with projections indicating a continued rise to 31.80 by 2030 (95% CI: 25.42–37.65; MAPE: 6.13%). In Cohort 1, the mean AAPC was higher in males (5.90; 95% CI: 4.25–7.56) than in females (3.60; 95% CI: 2.13–5.09). Comparable trends were observed in Cohort 2, with AAPCs of 4.37 (95% CI: 3.62–5.12) in males and 3.43 (95% CI: 2.48–4.39) in females. In the South (Census Region 3), Cohort 1 demonstrated a substantially higher mean APC of 6.59 (95% CI: 4.56–8.67) compared to 3.19 (95% CI: 2.28–4.12) in Cohort 2. Among Hispanics, Cohort 1 had a mean APC of 6.57 (95% CI: 1.12–12.31), compared to 4.06 (95% CI: 2.69–5.45) in Cohort 2. Among White individuals, Cohort 1 showed a higher APC of 5.49 (95% CI: 4.39–6.60) versus 4.30 (95% CI: 3.33–5.27) in Cohort 2.
Conclusion: Cohort 1 demonstrated higher mortality trends across multiple subgroups, indicating a disproportionate burden of mortality in this high-risk group. However, ARIMA projections suggest that while Cohort 1's trend declines by 2030, Cohort 2 will continue to rise, potentially surpassing Cohort 1.
More abstracts on this topic:
A Case Series of Papillary Fibroelastomas on the Coumadin ridge
Aboukhatwa Omar, Akiki Elias, Kurmann Reto, Larson Kathryn, Keeney Michael, Bois Melanie, Klarich Kyle
Acute Exposure to High PM2.5 Levels Increases the Risk of Late All-Cause Mortality in Patients with STEMIFathieh Sina, Tran Hao, Faour Amir, Pahn Reece, Long Mitchell, Tam Gladys, Figtree Gemma, Negishi Kazuaki, French John