Final ID: TAC138
Impact of Intensive Blood Pressure Control on Clinical Outcomes in Patients with Diabetes: A Meta-Analysis of Randomized Controlled Trials
Abstract Body: Background: There is no evidence from randomized trials to support a standard strategy of lowering systolic blood pressure below 140 mm Hg in persons with type 2 diabetes mellitus. We investigated whether intensive therapy targeting normal systolic pressure (i.e., <120 mm Hg) reduces major cardiovascular events in participants with type 2 diabetes at high risk for cardiovascular events.
Methods: We systematically searched PubMed, Embase and Cochrane databases for randomized controlled trials (RCTs) comparing the impact of intensive versus standard blood pressure control in patients with type 2 diabetes mellitus with the primary outcome of interest being all-cause mortality.
We pooled risk ratio and their 95% confidence intervals (CIs). We also examined heterogeneity using I2 statistics and studies with high heterogeneity were examined using the random-effect model.
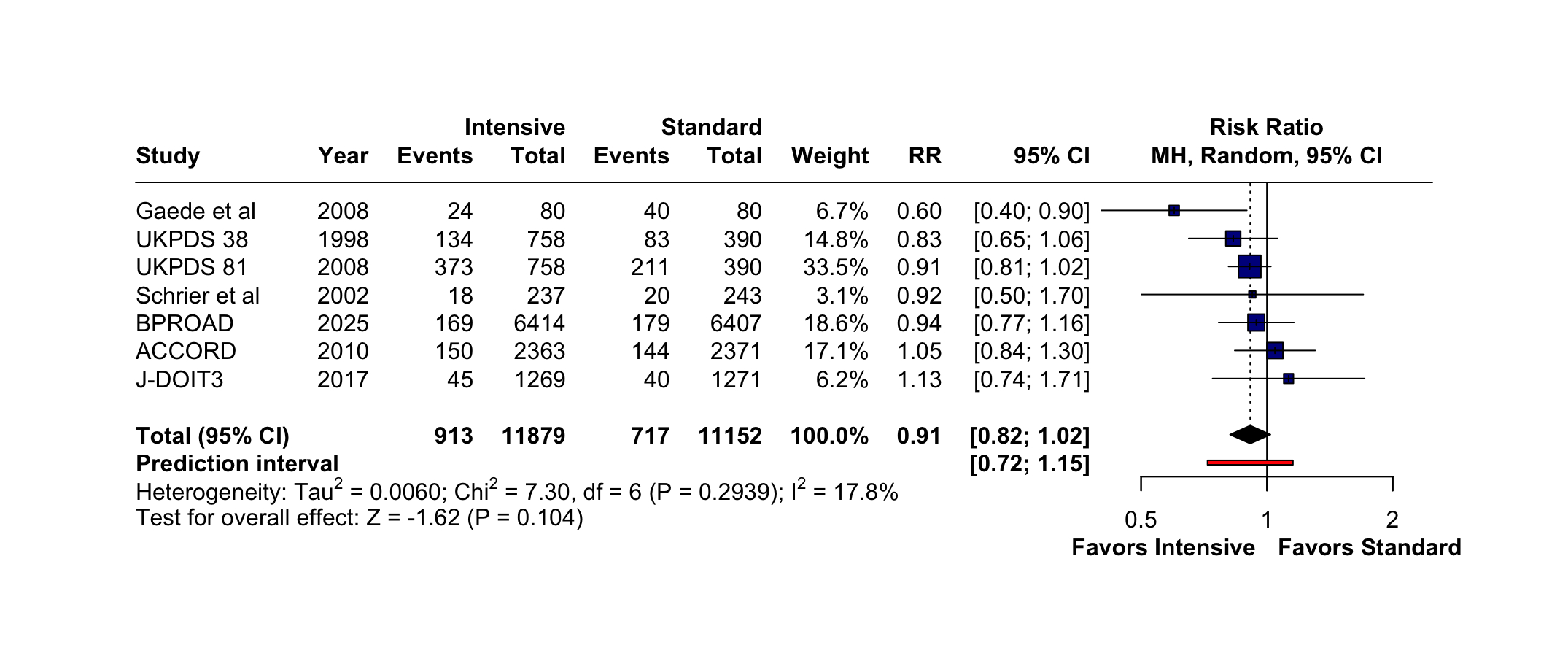
Results: We included 8 RCTs consisting of 23,121 patients with type 2 diabetes mellitus of which 11,926 (51.6%) had intensive blood pressure treatment while 11,195 (48.4%) had standard blood pressure treatment. The mean age of the included studies was 59.6 years and 56.6% were males. There were no significant differences between groups for all-cause mortality (RR = 0.91; 95% CI [0.82, 1.02]; I2 = 17.8%; p = 0.104; Figure 1), cardiovascular death (RR = 0.87; 95% CI [0.62, 1.23]; I2 = 35.6%; p = 0.427), heart failure (RR = 0.84; 95% CI [0.70, 1.00]; I2 = 0%; p = 0.045) and myocardial infarction (RR = 0.75; 95% CI [0.55, 1.03]; I2 = 57.1%; p = 0.077). However, intensive blood pressure control significantly reduced the incidence of stroke (RR = 0.56; 95% CI [0.41, 0.75]; I2 = 64.3%; p < 0.001) compared to standard treatment.
Conclusions: Intensive blood pressure control did not reduce all-cause mortality, cardiovascular death, heart failure and myocardial infarction despite reducing the incidence of stroke.
Methods: We systematically searched PubMed, Embase and Cochrane databases for randomized controlled trials (RCTs) comparing the impact of intensive versus standard blood pressure control in patients with type 2 diabetes mellitus with the primary outcome of interest being all-cause mortality.
We pooled risk ratio and their 95% confidence intervals (CIs). We also examined heterogeneity using I2 statistics and studies with high heterogeneity were examined using the random-effect model.
Results: We included 8 RCTs consisting of 23,121 patients with type 2 diabetes mellitus of which 11,926 (51.6%) had intensive blood pressure treatment while 11,195 (48.4%) had standard blood pressure treatment. The mean age of the included studies was 59.6 years and 56.6% were males. There were no significant differences between groups for all-cause mortality (RR = 0.91; 95% CI [0.82, 1.02]; I2 = 17.8%; p = 0.104; Figure 1), cardiovascular death (RR = 0.87; 95% CI [0.62, 1.23]; I2 = 35.6%; p = 0.427), heart failure (RR = 0.84; 95% CI [0.70, 1.00]; I2 = 0%; p = 0.045) and myocardial infarction (RR = 0.75; 95% CI [0.55, 1.03]; I2 = 57.1%; p = 0.077). However, intensive blood pressure control significantly reduced the incidence of stroke (RR = 0.56; 95% CI [0.41, 0.75]; I2 = 64.3%; p < 0.001) compared to standard treatment.
Conclusions: Intensive blood pressure control did not reduce all-cause mortality, cardiovascular death, heart failure and myocardial infarction despite reducing the incidence of stroke.
More abstracts on this topic:
30-day and one-year outcomes of patients with severe aortic stenosis after TAVI using Myval : A Meta-analysis
Hasabo Elfatih A., Sultan Sherif, Soliman Osama, A. Aboali Amira, Hemmeda Lina, Salah Alaa, Alrawa Salma S., Elgadi Ammar, Abdalmotalib Malaz, Yasir H Eissa Abdullatif, Mahmmoud Fadelallah Eljack Mohammed
Aspirin for Primary Prevention of Cardiovascular Events in Patients with Diabetes Mellitus: An Updated Systematic Review, Meta-Analysis & Trial Sequential Analysis of Randomized Controlled Trials post-ASCEND TrialPuthia Valappil Omer Mohammed, John M Rose, Mallikarjun Samanth, D Souza Leroy, Rongala Sai Anurag, Chakraborty Diya, Balarishnan Rojith, Kutty Shelby