Final ID: Su4006
Fractional flow reserve guided complete revascularization versus Culprit-only percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease. A meta-analysis of randomized controlled trials
Abstract Body (Do not enter title and authors here): Background: Data comparing the efficacy and safety of fractional flow reserve (FFR)-guided complete revascularization (CR) to culprit-only percutaneous coronary artery intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI) and multivessel coronary artery disease are limited.
Method: Pubmed, Embase and Cochrane were searched for randomized controlled trails (RCTs) comparing FFR-guided CR to Culprit-only PCI in patients with STEMI and multivessel CAD. A meta-analysis was performed on primary outcomes of major adverse cardiac events (MACE) and all-cause mortality. Heterogeneity was examined with I2 statistics. A random-effects model was used for outcomes with high heterogeneity.
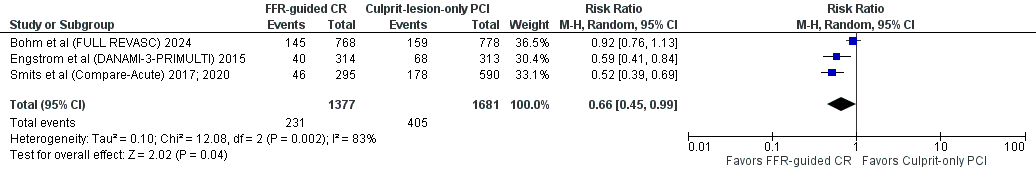
Results: We included 4 RCTs with 3173 patients comparing FFR-guided CR with culprit-only PCI in patients with STEMI and multivessel coronary artery diseases. The pooled results of the 4 RCTs showed that MACE (RR=0.66; 95% CI [0.45, 0.99]; p=0.01; 16.8% vs 24.1%), PCI revascularization (RR=0.50; 95% CI [0.37, 0.67]; p<0.00001; 13.1% vs 24.9%) and unplanned revascularization (RR=0.66; 95% CI [0.44, 0.99]; p=0.04; 8.7% vs 12.9%) were significantly reduced in the FFR-guided complete revascularization group compared to culprit-only PCI group.
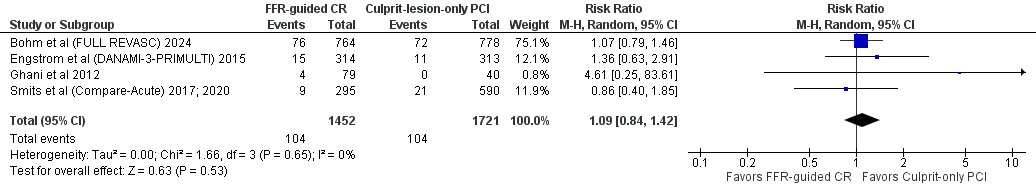
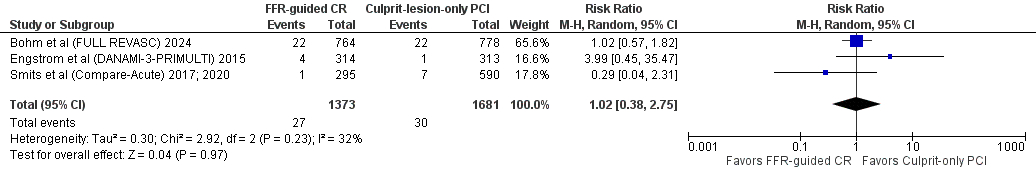
However, all-cause mortality (RR=1.09; 95% CI [0.84, 1.42]; p=0.53; 7.2% vs 6.0%), stroke (RR=1.02; 95% CI [0.38, 2.75]; p =0.97; 2.0% vs 1.8%), major bleeding (RR=0.95; 95% CI [0.54, 1.67]; p=0.87; 1.7% vs 1.7%), death from cardiovascular causes (RR=0.82; 95% CI [0.55, 1.21]; p=0.31; 3.1% vs 3.4%), MI (RR=1.09; 95% CI [0.60, 1.95]; p=0.78; 6.7% vs 6.4%), rehospitalization for HF (RR=0.72; 95% CI [0.44, 1.15]; p=0.17; 3.4% vs 5.3%), death from any cause or MI (RR=1.02; 95% CI [0.61, 1.71]; p=0.95; 14.9% vs 13.6%), any stent thrombosis (RR=1.42; 95% CI [0.35, 5.72]; p=0.62; 2.2% vs 1.4%), contrast induced nephropathy (RR=0.25; 95% CI [0.02, 2.79]; p=0.26), and CABG revascularization (RR=1.25; 95% CI [0.30, 5.15]; p=0.76) were not statistically different between groups.
Conclusion: Our meta-analysis suggests that FFR-guided CR is safe and has superior efficacy to Culprit-only PCI in patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease with significantly lowered incidence of MACE, PCI revascularization as well as unplanned or urgent revascularization. However, FFR-guided CR showed no beneficial effect on all-cause mortality, stroke, major bleeding and myocardial infarction.
Method: Pubmed, Embase and Cochrane were searched for randomized controlled trails (RCTs) comparing FFR-guided CR to Culprit-only PCI in patients with STEMI and multivessel CAD. A meta-analysis was performed on primary outcomes of major adverse cardiac events (MACE) and all-cause mortality. Heterogeneity was examined with I2 statistics. A random-effects model was used for outcomes with high heterogeneity.
Results: We included 4 RCTs with 3173 patients comparing FFR-guided CR with culprit-only PCI in patients with STEMI and multivessel coronary artery diseases. The pooled results of the 4 RCTs showed that MACE (RR=0.66; 95% CI [0.45, 0.99]; p=0.01; 16.8% vs 24.1%), PCI revascularization (RR=0.50; 95% CI [0.37, 0.67]; p<0.00001; 13.1% vs 24.9%) and unplanned revascularization (RR=0.66; 95% CI [0.44, 0.99]; p=0.04; 8.7% vs 12.9%) were significantly reduced in the FFR-guided complete revascularization group compared to culprit-only PCI group.
However, all-cause mortality (RR=1.09; 95% CI [0.84, 1.42]; p=0.53; 7.2% vs 6.0%), stroke (RR=1.02; 95% CI [0.38, 2.75]; p =0.97; 2.0% vs 1.8%), major bleeding (RR=0.95; 95% CI [0.54, 1.67]; p=0.87; 1.7% vs 1.7%), death from cardiovascular causes (RR=0.82; 95% CI [0.55, 1.21]; p=0.31; 3.1% vs 3.4%), MI (RR=1.09; 95% CI [0.60, 1.95]; p=0.78; 6.7% vs 6.4%), rehospitalization for HF (RR=0.72; 95% CI [0.44, 1.15]; p=0.17; 3.4% vs 5.3%), death from any cause or MI (RR=1.02; 95% CI [0.61, 1.71]; p=0.95; 14.9% vs 13.6%), any stent thrombosis (RR=1.42; 95% CI [0.35, 5.72]; p=0.62; 2.2% vs 1.4%), contrast induced nephropathy (RR=0.25; 95% CI [0.02, 2.79]; p=0.26), and CABG revascularization (RR=1.25; 95% CI [0.30, 5.15]; p=0.76) were not statistically different between groups.
Conclusion: Our meta-analysis suggests that FFR-guided CR is safe and has superior efficacy to Culprit-only PCI in patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease with significantly lowered incidence of MACE, PCI revascularization as well as unplanned or urgent revascularization. However, FFR-guided CR showed no beneficial effect on all-cause mortality, stroke, major bleeding and myocardial infarction.
More abstracts on this topic:
Abbreviated Ticagrelor-Based Dual Antiplatelet Therapy in Acute Coronary Syndrome: A Systematic Review and Meta-Analysis
Harmouch Wissam, Elbadawi Ayman, Thakker Ravi, Khalid Umair, Khalife Wissam, Kleiman Neal, Rangasetty Umamahesh, Kayani Waleed, Jneid Hani, Al Hemyari Bashar
Artificial Intelligence ECG-Extracted Features Predict Microvascular Obstruction in ST-segment Elevation Myocardial InfarctionTraverse Jay, Meyers Pendell, Sharkey Scott, Schwager Sarah, Stanberry Larissa, Herman Robert