Final ID: FR533
Association Between Postprandial Hypotension Determined by Ambulatory Blood Pressure Monitoring and Falls Among Older Adults with Hypertension Who Are Taking Antihypertensive Medication: Results from the AMBROSIA Study
Abstract Body: Background: Postprandial hypotension (PPH), defined as a large decline in blood pressure (BP) after a meal, has typically been assessed using BP measured in a clinic setting. However, evidence regarding PPH evaluated outside the clinic and under usual daily meal conditions is scarce. We evaluated PPH and fall risk using out-of-office BP monitoring, ambulatory BP monitoring (ABPM), among community-dwelling older adults with hypertension who were taking antihypertensive medications.
Hypothesis: PPH determined by ABPM is associated with an increased risk of falls among older adults taking antihypertensive medication.
Methods: The AMBulatoRy blood preSsure In older Adults (AMBROSIA) study enrolled a prospective cohort of adults aged ≥65 years who were taking antihypertensive medication, from an integrated healthcare system in the United States, to examine the utility of ABPM for identifying fall risk. Participants underwent 24-hour ABPM at baseline. Data on falls during the subsequent 12-month follow-up period were prospectively collected each month using falls calendars. Preprandial systolic BP (SBP) was defined as the mean SBP during the 1 hour before a meal, and postprandial SBP as the minimum SBP during the 2 hours after the meal. Systolic PPH was defined as either a decline from preprandial to postprandial SBP of ≥20 mm Hg, or a postprandial SBP of ≤90 mm Hg when preprandial SBP was ≥100 mm Hg for any meal.
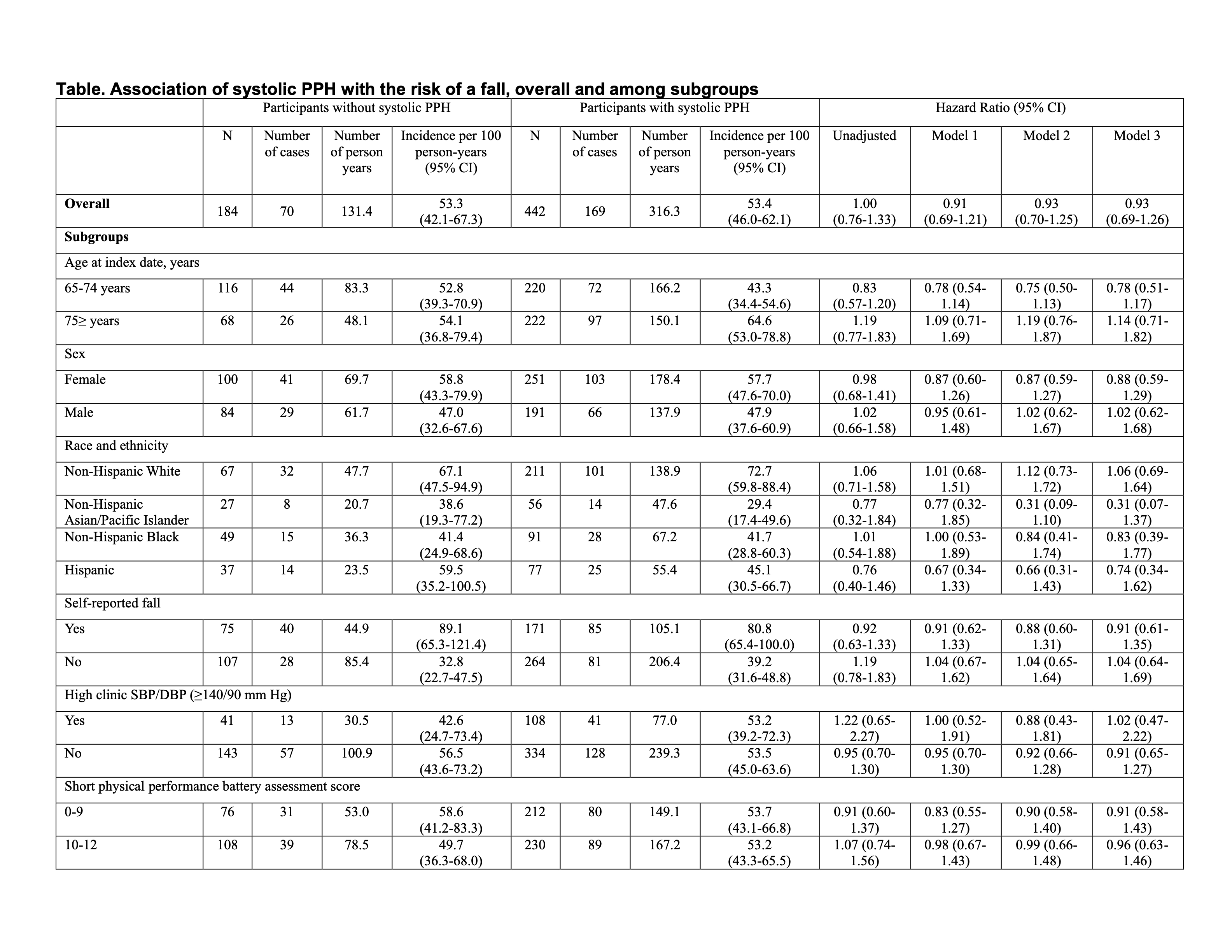
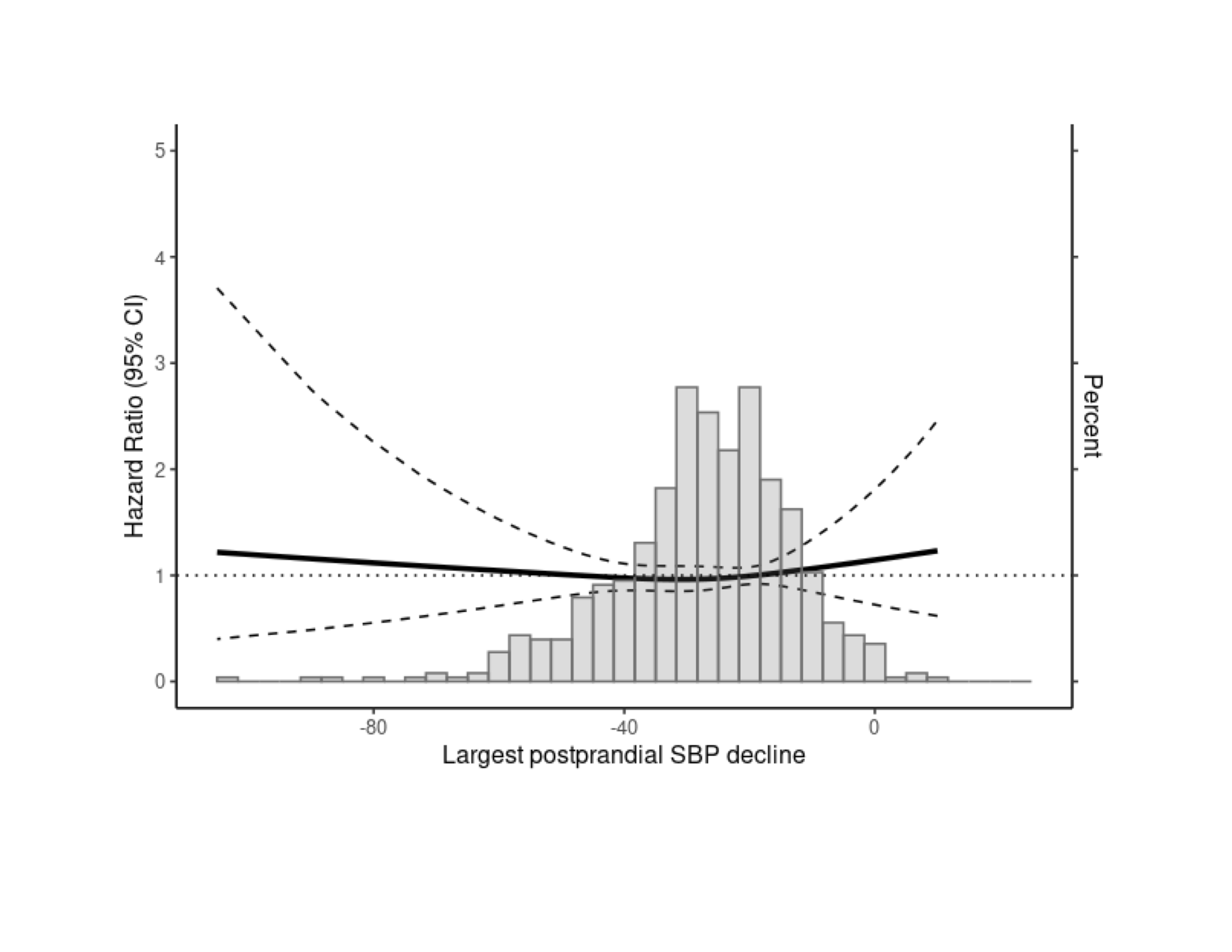
Results: Among 626 participants (mean ± SD age: 74.6 ± 6.2 years; 56.1% female; mean awake SBP: 134.6 ± 13.7 mm Hg), 442 (70.6%) had systolic PPH. During the 12-month follow-up, falls occurred in 38.0% and 38.2% of participants with and without systolic PPH, respectively. In a Cox regression analysis controlling for several potential demographic and clinical risk factors, systolic PPH was not associated with an increased risk of falls compared to those without systolic PPH in the overall study population (adjusted HR: 0.93, 95% CI: 0.69-1.26), nor in subgroups defined by age, sex, race/ethnicity, history of falls, or clinic BP (Table). A restricted cubic spline analysis revealed no association between greater postprandial SBP decline and fall risk (Figure).
Conclusions: Systolic PPH determined using ABPM was common among community-dwelling older adults taking antihypertensive medication, but it was not associated with an increased risk of falls.
Hypothesis: PPH determined by ABPM is associated with an increased risk of falls among older adults taking antihypertensive medication.
Methods: The AMBulatoRy blood preSsure In older Adults (AMBROSIA) study enrolled a prospective cohort of adults aged ≥65 years who were taking antihypertensive medication, from an integrated healthcare system in the United States, to examine the utility of ABPM for identifying fall risk. Participants underwent 24-hour ABPM at baseline. Data on falls during the subsequent 12-month follow-up period were prospectively collected each month using falls calendars. Preprandial systolic BP (SBP) was defined as the mean SBP during the 1 hour before a meal, and postprandial SBP as the minimum SBP during the 2 hours after the meal. Systolic PPH was defined as either a decline from preprandial to postprandial SBP of ≥20 mm Hg, or a postprandial SBP of ≤90 mm Hg when preprandial SBP was ≥100 mm Hg for any meal.
Results: Among 626 participants (mean ± SD age: 74.6 ± 6.2 years; 56.1% female; mean awake SBP: 134.6 ± 13.7 mm Hg), 442 (70.6%) had systolic PPH. During the 12-month follow-up, falls occurred in 38.0% and 38.2% of participants with and without systolic PPH, respectively. In a Cox regression analysis controlling for several potential demographic and clinical risk factors, systolic PPH was not associated with an increased risk of falls compared to those without systolic PPH in the overall study population (adjusted HR: 0.93, 95% CI: 0.69-1.26), nor in subgroups defined by age, sex, race/ethnicity, history of falls, or clinic BP (Table). A restricted cubic spline analysis revealed no association between greater postprandial SBP decline and fall risk (Figure).
Conclusions: Systolic PPH determined using ABPM was common among community-dwelling older adults taking antihypertensive medication, but it was not associated with an increased risk of falls.
More abstracts on this topic:
2 Dimensional Echocardiography versus 3 Dimentional Echocardiography to Assess Right Ventricular Function in Pulmonary Hypertension: A Systematic Review
Chaudhry Waleed Razzaq, Hajj Fatima, Bathula Satyamedha, Meghji Mohammed Askari, Pasupuleti Hemalatha, Kiyani Madiha, Shah Syeda Simrah, Neelakantan Ramaswamy Sanathanan, Mirzaeidizaji Nakisa, St. Jacques Jahnoy, Khan Khalil Ullah, Veluchamy Elakkiya, Jesse Joshanna
Cigar smoking and better quality of life positively impact cigarette smoking cessation in adults: Findings from the Population Assessment of Tobacco and Health Study, a national longitudinal cohort studyMajeed Ban, Kaplan Bekir, Ketchem Justin, Walsh David