Final ID: FR463
Associations Between Shared Decision-Making and Adherence to High Blood Pressure Therapy in Adults with Cardiometabolic Multimorbidity: The LINKED-HEARTS Program
Abstract Body: Introduction: Shared decision-making (SDM) is recommended to support patient-centered care and improve blood pressure (BP) control. While adherence to high BP therapy (including medication adherence, sodium intake, and appointment keeping) are key hypertension self-care practices, the relationship between SDM and adherence to high BP therapy remains understudied.
Objective: To examine the associations between SDM and adherence to high BP therapy in a Cardiometabolic Health Program LINKED with Community Health WorkErs and Mobile HeAlth TelemonitoRing To reduce Health DisparitieS, the “LINKED-HEARTS” Program.
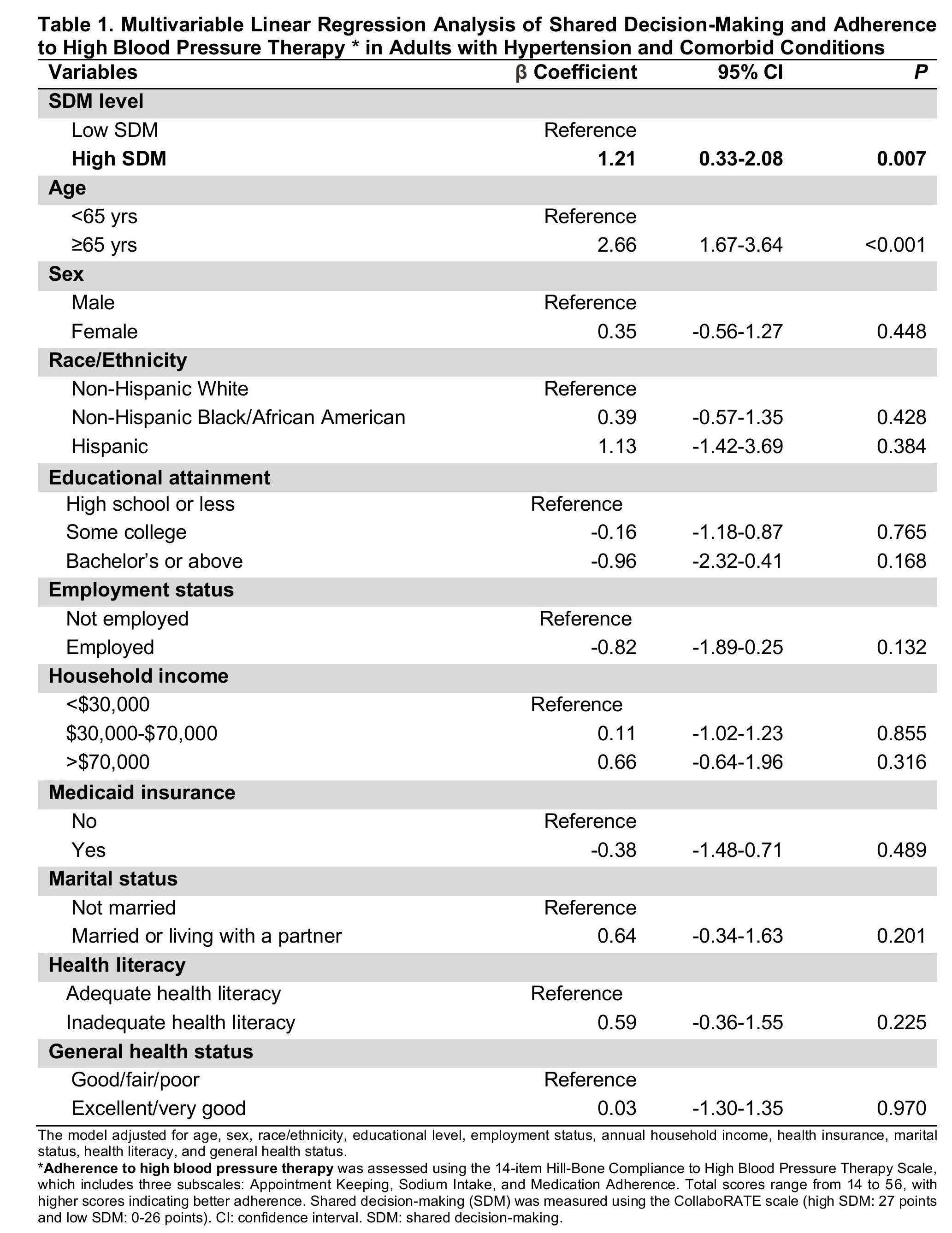
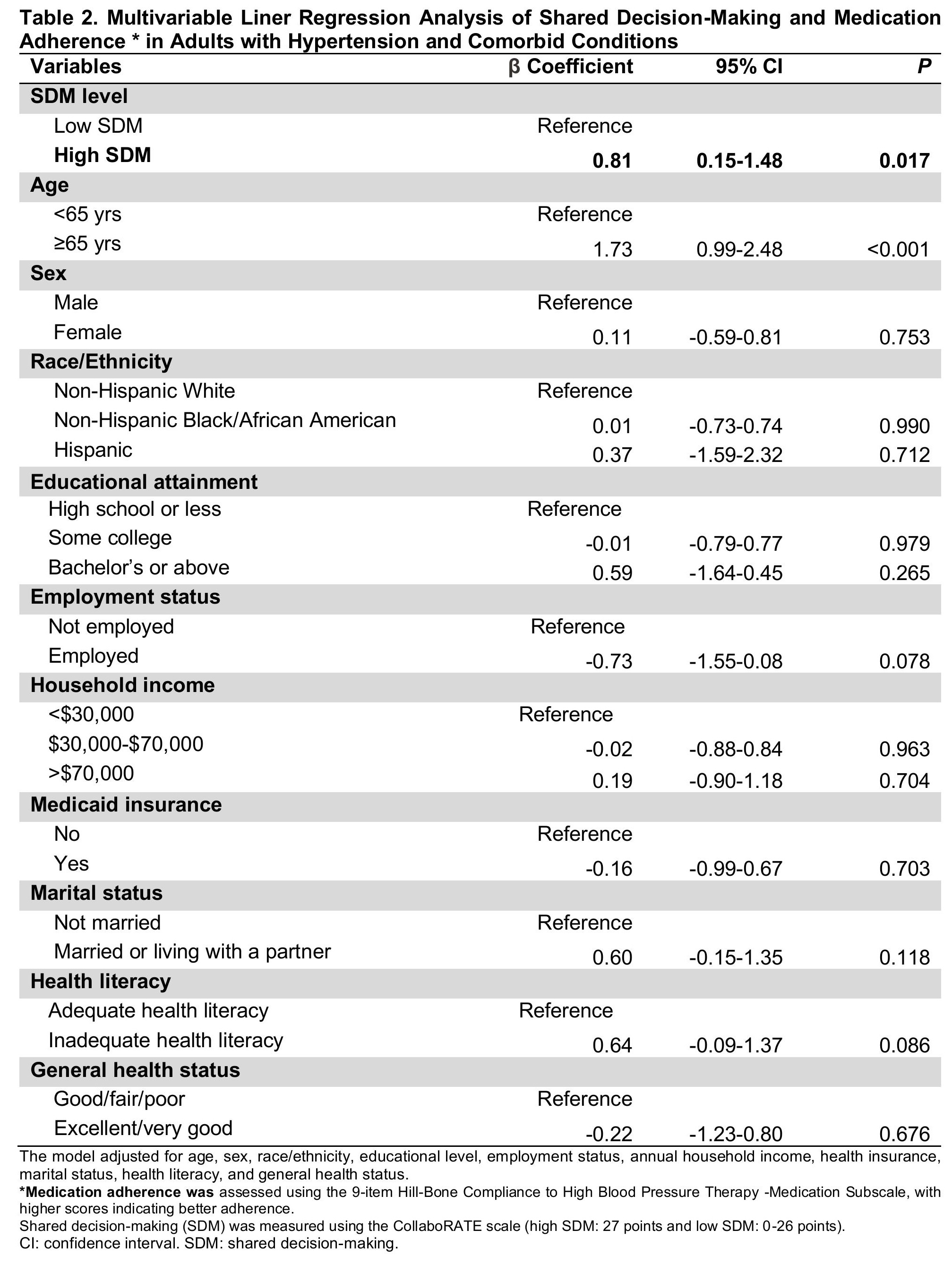
Method: This cross-sectional analysis was conducted using baseline data from the LINKED-HEARTS Program, an ongoing cluster randomized clinical trial of adults with hypertension and diabetes or chronic kidney disease. The exposure of interest was SDM, measured using the CollaboRATE scale (high SDM: 27 points and low SDM: 0-26 points). The outcome of interest was adherence to high BP therapy, assessed using the Hill-Bone Compliance to High BP Therapy Scale (HB-HBP), which includes three subscales: Medication Adherence, Appointment Keeping, and Sodium Intake. Total HB-HBP scores range from 14 to 56, with higher scores indicating better adherence to high BP therapy. To examine the association between SDM and adherence to high BP therapy (overall HB-HBP scale) and medication adherence (HB-HBP medication adherence subscale). We conducted two multivariable linear regression models adjusting for age, sex, race/ethnicity, educational level, employment status, annual household income, health insurance, marital status, health literacy, and general health status.
Results: The study included 333 adults with hypertension and comorbid conditions, with mean age of 62.8 years (±SD 12.3), of whom 63% were female and 64% were non-Hispanic Black adults. Mean score of the HB-HBP was 50.8 (±SD 3.9), and 39.4% reported high SDM. High SDM was significantly associated with greater adherence to high BP therapy (overall HB-HBP: β=1.21, 95% CI: 0.33-2.08, P=0.007) (Table 1) and medication adherence (HB-HBP medication adherence subscale: β=0.81, 95% CI: 0.15-1.48, P=0.017) (Table 2).
Conclusion: High SDM was associated with greater adherence to high BP therapy and medication among adults with cardiometabolic multimorbidity. Future research should explore strategies to enhance SDM and whether enhancing SDM can improve BP control by promoting medication adherence.
Objective: To examine the associations between SDM and adherence to high BP therapy in a Cardiometabolic Health Program LINKED with Community Health WorkErs and Mobile HeAlth TelemonitoRing To reduce Health DisparitieS, the “LINKED-HEARTS” Program.
Method: This cross-sectional analysis was conducted using baseline data from the LINKED-HEARTS Program, an ongoing cluster randomized clinical trial of adults with hypertension and diabetes or chronic kidney disease. The exposure of interest was SDM, measured using the CollaboRATE scale (high SDM: 27 points and low SDM: 0-26 points). The outcome of interest was adherence to high BP therapy, assessed using the Hill-Bone Compliance to High BP Therapy Scale (HB-HBP), which includes three subscales: Medication Adherence, Appointment Keeping, and Sodium Intake. Total HB-HBP scores range from 14 to 56, with higher scores indicating better adherence to high BP therapy. To examine the association between SDM and adherence to high BP therapy (overall HB-HBP scale) and medication adherence (HB-HBP medication adherence subscale). We conducted two multivariable linear regression models adjusting for age, sex, race/ethnicity, educational level, employment status, annual household income, health insurance, marital status, health literacy, and general health status.
Results: The study included 333 adults with hypertension and comorbid conditions, with mean age of 62.8 years (±SD 12.3), of whom 63% were female and 64% were non-Hispanic Black adults. Mean score of the HB-HBP was 50.8 (±SD 3.9), and 39.4% reported high SDM. High SDM was significantly associated with greater adherence to high BP therapy (overall HB-HBP: β=1.21, 95% CI: 0.33-2.08, P=0.007) (Table 1) and medication adherence (HB-HBP medication adherence subscale: β=0.81, 95% CI: 0.15-1.48, P=0.017) (Table 2).
Conclusion: High SDM was associated with greater adherence to high BP therapy and medication among adults with cardiometabolic multimorbidity. Future research should explore strategies to enhance SDM and whether enhancing SDM can improve BP control by promoting medication adherence.
More abstracts on this topic:
3CPR Best Abstract Award: The pathogenic role of ADAMTS13 deficiency in Chronic Thromboembolic Pulmonary Hypertension
Wu Zhijian, Zheng X. Long, Zheng Liang
Co-Design and Development of a Web-Based Decision Aid to Support Team-Based Shared Decision-Making to Advance Cardiovascular Health: A Mixed Method StudyChen Yuling, Adomako Nana, Orellana Andrea, Benjasirisan Chitchanok, Lewis Krystina, Dennison Himmelfarb Cheryl