Final ID: Mo2038
Trends in Statin Prescribing for Primary Prevention in the United States
Abstract Body (Do not enter title and authors here): Introduction
Cardiovascular disease remains the leading cause of morbidity and death in the US, with coronary disease being the leading cause of death. Statins are a cornerstone of preventive cardiology practice, and their initiation for the primary prevention of atherosclerotic cardiovascular disease (ASCVD) when appropriate is of utmost importance. The present study explored statin prescribing trends for primary prevention of ASCVD in the US.
Methods
We conducted a pooled cross-sectional analysis using EHRs from Epic Cosmos, an integrated, deduplicated database including more than 290 million patients across the US. Patients eligible for statin therapy for primary prevention between 1/2017 and 12/2024, according to current guidelines, were included (adults aged 40-75 years with a 10-year ASCVD risk ≥ 7.5%, adults ≥40 years with DM (HbA1c >6.5%), or individuals with an LDL cholesterol ≥190 mg/dL). Patients with established ASCVD (ACS, stable angina, PCI /CABG, PAD, or CVA) were excluded. National prescribing trends were analyzed.
Results
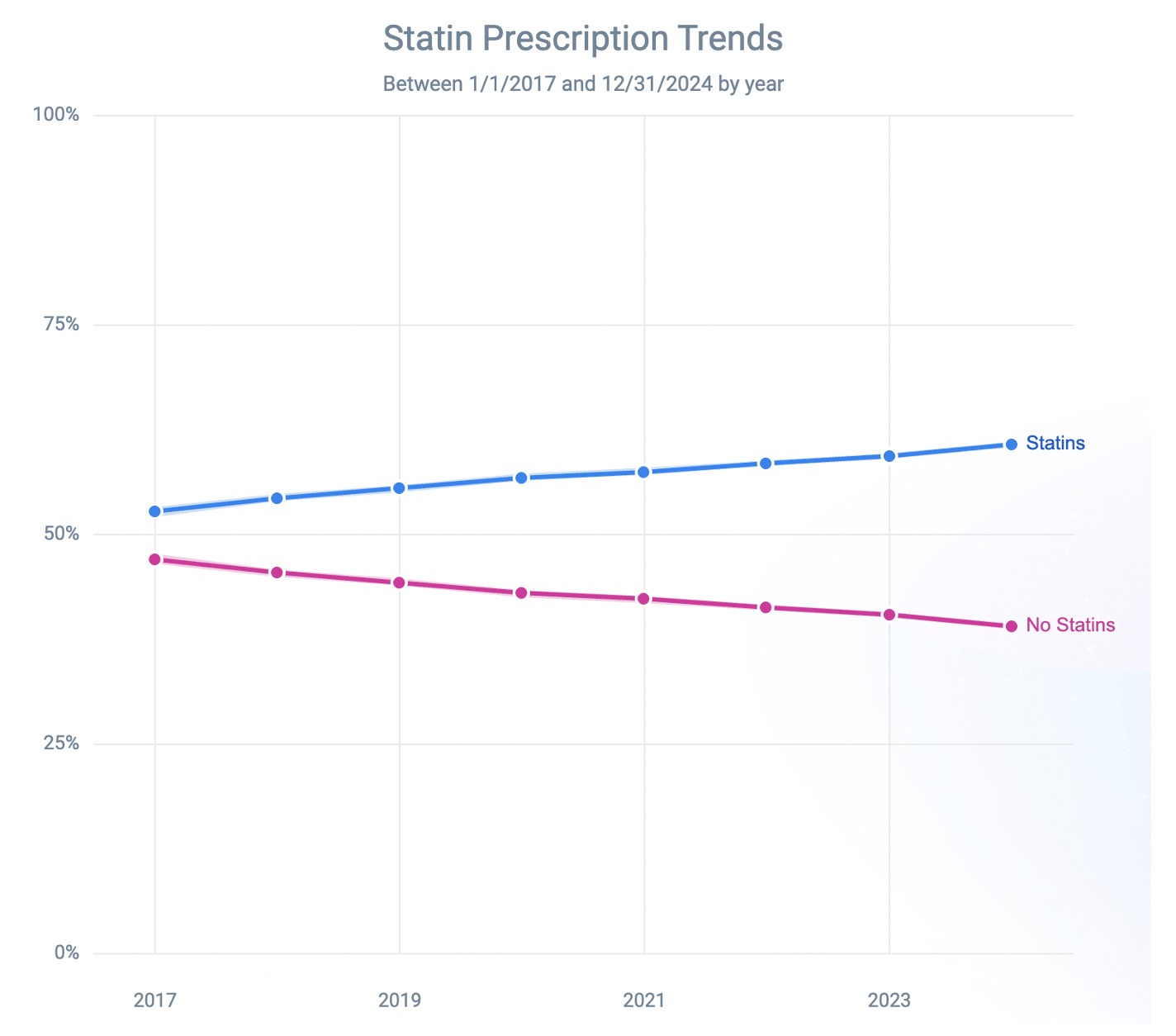
A total of 15,770,021 patients met inclusion criteria. Among them, 9,377,988 (59.5%) were prescribed a statin, while 6,392,033 (40.5%) were not. Of those prescribed a statin, 3,485,418 (37.2%) were on a high-intensity statin. Baseline characteristics were generally similar between patients prescribed statins and those who were not, including average age (67 ± 20 vs. 66 ± 19 years), sex distribution (49.9% vs. 50.4% female), and race/ethinicity (White: 76.0% vs. 74.6%; Black: 16.0% vs. 16.1%; Hispanic: 8.6% vs. 7.9%). The average Area Deprivation Index was comparable between both groups (53 each). On trend analysis, the rate of statin prescriptions for primary prevention among eligible patients increased significantly from 52.8% in 2017 (95% CI: 52.3–53.2) to 62.8% in 2024 (95% CI: 62.5–63.1) (p < 0.001) (Figure 1). In subgroup analysis, 64.5% of adults aged 40–75 years with a 10-year ASCVD risk ≥ 7.5%, 60.4% of adults ≥40 years with DM, and 63.3% of patients with LDL ≥ 190 mg/dL were prescribed a statin in 2024. The difference in statin prescribing rates across the subgroups was statistically significant (p < 0.001).
Conclusions
Statin prescribing for primary prevention has increased significantly in the US over the past decade, yet almost 40% of eligible patients remained untreated in 2024. These findings highlight ongoing gaps in preventive care and the need for enhanced implementation of guideline-directed statin therapy.
Cardiovascular disease remains the leading cause of morbidity and death in the US, with coronary disease being the leading cause of death. Statins are a cornerstone of preventive cardiology practice, and their initiation for the primary prevention of atherosclerotic cardiovascular disease (ASCVD) when appropriate is of utmost importance. The present study explored statin prescribing trends for primary prevention of ASCVD in the US.
Methods
We conducted a pooled cross-sectional analysis using EHRs from Epic Cosmos, an integrated, deduplicated database including more than 290 million patients across the US. Patients eligible for statin therapy for primary prevention between 1/2017 and 12/2024, according to current guidelines, were included (adults aged 40-75 years with a 10-year ASCVD risk ≥ 7.5%, adults ≥40 years with DM (HbA1c >6.5%), or individuals with an LDL cholesterol ≥190 mg/dL). Patients with established ASCVD (ACS, stable angina, PCI /CABG, PAD, or CVA) were excluded. National prescribing trends were analyzed.
Results
A total of 15,770,021 patients met inclusion criteria. Among them, 9,377,988 (59.5%) were prescribed a statin, while 6,392,033 (40.5%) were not. Of those prescribed a statin, 3,485,418 (37.2%) were on a high-intensity statin. Baseline characteristics were generally similar between patients prescribed statins and those who were not, including average age (67 ± 20 vs. 66 ± 19 years), sex distribution (49.9% vs. 50.4% female), and race/ethinicity (White: 76.0% vs. 74.6%; Black: 16.0% vs. 16.1%; Hispanic: 8.6% vs. 7.9%). The average Area Deprivation Index was comparable between both groups (53 each). On trend analysis, the rate of statin prescriptions for primary prevention among eligible patients increased significantly from 52.8% in 2017 (95% CI: 52.3–53.2) to 62.8% in 2024 (95% CI: 62.5–63.1) (p < 0.001) (Figure 1). In subgroup analysis, 64.5% of adults aged 40–75 years with a 10-year ASCVD risk ≥ 7.5%, 60.4% of adults ≥40 years with DM, and 63.3% of patients with LDL ≥ 190 mg/dL were prescribed a statin in 2024. The difference in statin prescribing rates across the subgroups was statistically significant (p < 0.001).
Conclusions
Statin prescribing for primary prevention has increased significantly in the US over the past decade, yet almost 40% of eligible patients remained untreated in 2024. These findings highlight ongoing gaps in preventive care and the need for enhanced implementation of guideline-directed statin therapy.
More abstracts on this topic:
Adding a polygenic risk score to the PREVENT clinical risk tool significantly improves cardiovascular risk prediction
Euesden Jack, Absher Devin, Iribarren Carlos, Riveros-mckay Fernando, Rana Jamal, Rowell Sarah, Neogi Arpita, Harrison Seamus, Weale Michael, Donnelly Peter
A Delayed Diagnosis of Anti-HMG-CoA Reductase Immune-Mediated Necrotizing MyopathyJadhav Reshma, Shekar Arush, Westenhaver Zack, Skandhan Amith