Final ID: Su2090
Evaluating Remote Versus Clinic-Based Follow-Up in Postpartum Hypertension: A Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here): Introduction
Hypertensive disorders of pregnancy (HDP) contribute to postpartum complications and readmissions. Remote blood pressure monitoring (RBPM) offers an effective alternative for tracking postpartum health. However, evidence on its benefits compared to OB-GYN clinic visits is limited. This study aims to determine whether remote postpartum blood pressure monitoring improves clinical outcomes over traditional follow-ups for individuals with a history of hypertensive disorders during pregnancy.
Methods
A literature search was conducted following PRISMA guidelines across PubMed, Google Scholar, and Embase for studies on postpartum outcomes using RBPM via text, telehealth, home-based platforms, or clinic care. Primary outcomes were blood pressure control, follow-up adherence, and hospital readmissions. Secondary outcomes included blood pressure reporting, emergency room visits, and patient satisfaction. Random-effects models analyzed pooled proportions with 95% confidence intervals (CI). Statistical significance was set at p<0.05.
Results
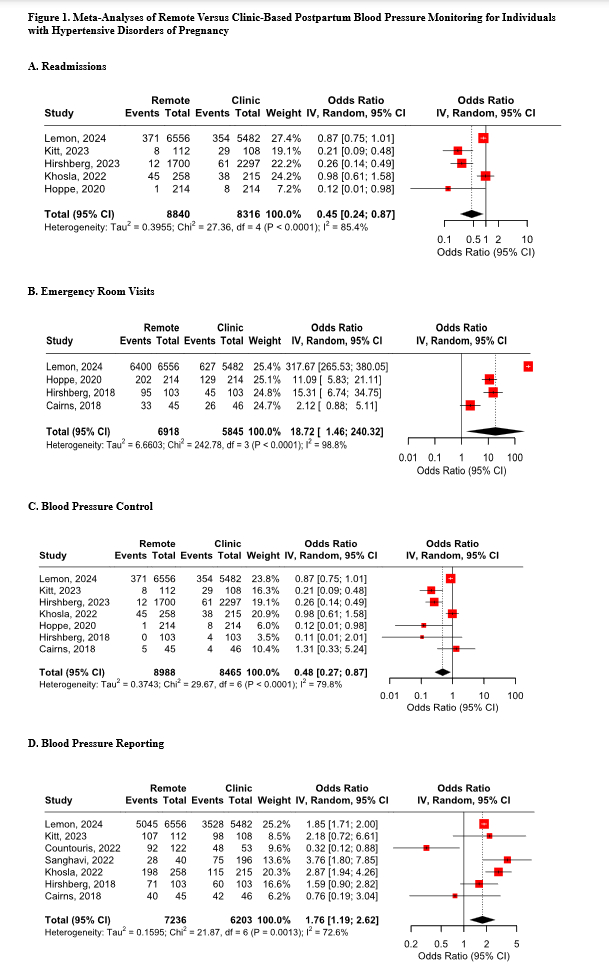
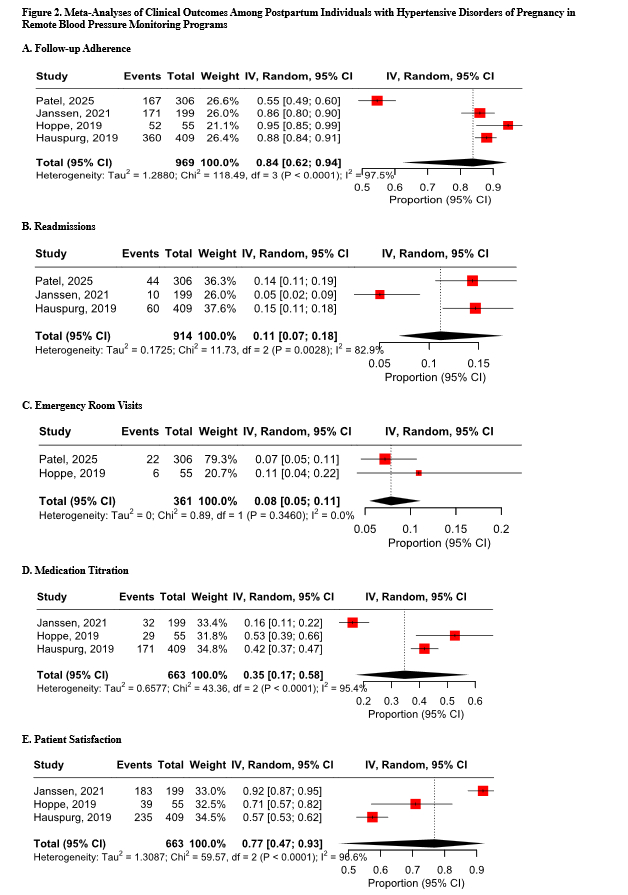
Thirteen studies included over 18,833 postpartum individuals with HDP. Compared with clinic-based care, remote monitoring significantly reduced readmissions (OR: 0.45; 95% CI: 0.24-0.87; p=0.017), improved blood pressure control (<140/90mmHg) (OR: 0.48; 95% CI: 0.27-0.87; p=0.016), and increased blood pressure reporting (OR: 1.76; 95% CI: 1.19-2.62; p=0.005) (Fig 1). However, remote monitoring was associated with increased emergency room visits (OR: 18.72; 95% CI: 1.46-240.32; p=0.025), possibly indicating earlier triage. Single-arm analyses (Fig 2) of RBPM cohorts reported high follow-up adherence (OR: 14.63; 95% CI: 0.88-242.19; p=0.061), low readmission rates (OR: 0.13; 95% CI: 0.07-0.22; p<0.001), and low emergency visit rates (OR: 0.08; 95% CI: 0.05-0.11; p<0.001). Medication titration was moderate (OR: 0.52; 95% CI: 0.39-0.66; p<0.001), and patient satisfaction was high (OR: 2.95; 95% CI: 0.61-14.39; p=0.179). Moderate to High heterogeneity was observed among all the analyses.
Conclusion
RBPM improves postpartum management by enhancing follow-up adherence, control, and reporting, while lowering readmission rates. Increased emergency visits indicate timely detection rather than negative outcomes. Further research is needed to assess the impact of socioeconomic factors, insurance coverage, and access to care on the implementation and effectiveness of interventions across diverse populations.
Hypertensive disorders of pregnancy (HDP) contribute to postpartum complications and readmissions. Remote blood pressure monitoring (RBPM) offers an effective alternative for tracking postpartum health. However, evidence on its benefits compared to OB-GYN clinic visits is limited. This study aims to determine whether remote postpartum blood pressure monitoring improves clinical outcomes over traditional follow-ups for individuals with a history of hypertensive disorders during pregnancy.
Methods
A literature search was conducted following PRISMA guidelines across PubMed, Google Scholar, and Embase for studies on postpartum outcomes using RBPM via text, telehealth, home-based platforms, or clinic care. Primary outcomes were blood pressure control, follow-up adherence, and hospital readmissions. Secondary outcomes included blood pressure reporting, emergency room visits, and patient satisfaction. Random-effects models analyzed pooled proportions with 95% confidence intervals (CI). Statistical significance was set at p<0.05.
Results
Thirteen studies included over 18,833 postpartum individuals with HDP. Compared with clinic-based care, remote monitoring significantly reduced readmissions (OR: 0.45; 95% CI: 0.24-0.87; p=0.017), improved blood pressure control (<140/90mmHg) (OR: 0.48; 95% CI: 0.27-0.87; p=0.016), and increased blood pressure reporting (OR: 1.76; 95% CI: 1.19-2.62; p=0.005) (Fig 1). However, remote monitoring was associated with increased emergency room visits (OR: 18.72; 95% CI: 1.46-240.32; p=0.025), possibly indicating earlier triage. Single-arm analyses (Fig 2) of RBPM cohorts reported high follow-up adherence (OR: 14.63; 95% CI: 0.88-242.19; p=0.061), low readmission rates (OR: 0.13; 95% CI: 0.07-0.22; p<0.001), and low emergency visit rates (OR: 0.08; 95% CI: 0.05-0.11; p<0.001). Medication titration was moderate (OR: 0.52; 95% CI: 0.39-0.66; p<0.001), and patient satisfaction was high (OR: 2.95; 95% CI: 0.61-14.39; p=0.179). Moderate to High heterogeneity was observed among all the analyses.
Conclusion
RBPM improves postpartum management by enhancing follow-up adherence, control, and reporting, while lowering readmission rates. Increased emergency visits indicate timely detection rather than negative outcomes. Further research is needed to assess the impact of socioeconomic factors, insurance coverage, and access to care on the implementation and effectiveness of interventions across diverse populations.
More abstracts on this topic:
Center-Based, Home-Based, and Technology-Enhanced Cardiac Rehabilitation Equally Reduce Mortality Risk in Veterans
Shah Amit, Li Louis, Aggarwal Vinod, Zafari Abarmard, Park Linda, Harzand Arash
Presenting Signs and Symptoms of Maternal Stroke by Stroke Type: a Multicenter, Retrospective Case SeriesShang Catherine, Shields Andrea, Holl Jane, Prabhakaran Shyam, Miller Eliza, Haghighi Noora, Bourscheid Raeann, Romo Elida, Seitz Alison, Shapouran Sara, Mamer Lauren, Meurer William, Liberman Ava