Final ID: MP588
Discordance Between CAC Scoring and PREVENT Risk Estimates in Primary Prevention
Abstract Body (Do not enter title and authors here): Background
CAC scoring is a validated tool in primary prevention that stratifies cardiovascular risk and guides treatment decisions. The PREVENT algorithm uses clinical and sociodemographic inputs to estimate future CVD, ASCVD, and HF risk. While CAC and PREVENT offer categorical risk estimates, the degree to which PREVENT identifies risk in individuals with imaging-confirmed subclinical disease is understudied. Because CAC reflects active plaque burden at testing, an underestimation from PREVENT holds great clinical weight.
Methods
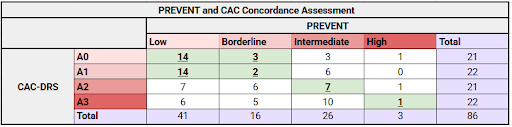
A dual-center study reviewed patients who underwent CAC scoring between January and May 2025. The inclusion criteria were a reported CAC, no documented ASCVD diagnosis based on ICD-10 codes and manual review, and appropriate input data required by PREVENT. Of the 184 patients reviewed, 86 met all criteria. CAC burden was categorized using CAC-DRS classifications: A0 (0; low), A1 (1–99; mild), A2 (100–299; moderate), and A3 (≥300; severe). PREVENT 10-year ASCVD risk was stratified as Low (<5%), Borderline (5–7.4%), Intermediate (7.5–19.9%), or High (≥20%). A "hit" was defined as a classification by PREVENT that aligned with the expected CAC-DRS category: Low or Borderline for A0 and A1, Intermediate for A2, and High for A3. This approach accounted for appropriate future risk estimation while emphasizing underestimating in patients with moderate to severe CAC scores.
Results
The CAC score was A0 in 24.4% (21/86), A1 in 25.6% (22/86), A2 in 24.4% (21/86), and A3 in 25.6% (22/86). PREVENT stratified patients as low risk in 47.7% (41/86), borderline in 18.6% (16/86), intermediate in 30.2% (26/86), and high in 3.5% (3/86). The hit rate in the A0 and A1 groups was 81.0% (17/21) and 72.7% (16/22), respectively. However, only 33.3% (7/21) of A2 and 4.5% (1/22) of A3 were a hit. In total, 52.3% (45/86) of patients were missed by PREVENT, indicating a notable discrepancy.
For high-risk patients, 79.1% (34/43) with A2 or A3 CAC burden were underestimated by PREVENT. However, the association between CAC burden and PREVENT-predicted risk was insignificant (Chi-square = 12.81, df = 9, p = 0.171), likely due to the limited patients in higher-risk PREVENT categories.
Conclusion
Among patients with moderate to severe CAC burden, PREVENT frequently assigned low or borderline 10-year ASCVD risk estimates. While insignificant, these findings warrant further validation of PREVENT's role in clinical workflows through follow-up studies with a larger n.
CAC scoring is a validated tool in primary prevention that stratifies cardiovascular risk and guides treatment decisions. The PREVENT algorithm uses clinical and sociodemographic inputs to estimate future CVD, ASCVD, and HF risk. While CAC and PREVENT offer categorical risk estimates, the degree to which PREVENT identifies risk in individuals with imaging-confirmed subclinical disease is understudied. Because CAC reflects active plaque burden at testing, an underestimation from PREVENT holds great clinical weight.
Methods
A dual-center study reviewed patients who underwent CAC scoring between January and May 2025. The inclusion criteria were a reported CAC, no documented ASCVD diagnosis based on ICD-10 codes and manual review, and appropriate input data required by PREVENT. Of the 184 patients reviewed, 86 met all criteria. CAC burden was categorized using CAC-DRS classifications: A0 (0; low), A1 (1–99; mild), A2 (100–299; moderate), and A3 (≥300; severe). PREVENT 10-year ASCVD risk was stratified as Low (<5%), Borderline (5–7.4%), Intermediate (7.5–19.9%), or High (≥20%). A "hit" was defined as a classification by PREVENT that aligned with the expected CAC-DRS category: Low or Borderline for A0 and A1, Intermediate for A2, and High for A3. This approach accounted for appropriate future risk estimation while emphasizing underestimating in patients with moderate to severe CAC scores.
Results
The CAC score was A0 in 24.4% (21/86), A1 in 25.6% (22/86), A2 in 24.4% (21/86), and A3 in 25.6% (22/86). PREVENT stratified patients as low risk in 47.7% (41/86), borderline in 18.6% (16/86), intermediate in 30.2% (26/86), and high in 3.5% (3/86). The hit rate in the A0 and A1 groups was 81.0% (17/21) and 72.7% (16/22), respectively. However, only 33.3% (7/21) of A2 and 4.5% (1/22) of A3 were a hit. In total, 52.3% (45/86) of patients were missed by PREVENT, indicating a notable discrepancy.
For high-risk patients, 79.1% (34/43) with A2 or A3 CAC burden were underestimated by PREVENT. However, the association between CAC burden and PREVENT-predicted risk was insignificant (Chi-square = 12.81, df = 9, p = 0.171), likely due to the limited patients in higher-risk PREVENT categories.
Conclusion
Among patients with moderate to severe CAC burden, PREVENT frequently assigned low or borderline 10-year ASCVD risk estimates. While insignificant, these findings warrant further validation of PREVENT's role in clinical workflows through follow-up studies with a larger n.
More abstracts on this topic:
A 50% or Greater Reduction in LDL-Cholesterol Is Associated with Improved Long-Term Outcomes and Lower Health Care Utilization After Myocardial Infarction - a SWEDEHEART study
Reitan Christian, Watanabe Alexandre, Bash Lori, Galvain Thibaut, Arnet Urs, Jernberg Tomas
3-Minute Heart Health App: A Feasibility StudyAbdulkarim Iya, Metzger Joseph, Stovitz Steven, Van't Hof Jeremy