Final ID: MP1938
Right Atrial Perforation and Cardiac Tamponade: A Rare Complication of Femoral Hemodialysis Catheter Exchange
Abstract Body (Do not enter title and authors here): Introduction: Right atrial perforation resulting in cardiac tamponade is a rare but life-threatening complication of hemodialysis catheter placement. While this is recognized with superior central venous access, perforation originating from a femoral hemodialysis catheter is exceedingly uncommon. We present a case of acute cardiac tamponade secondary to right atrial perforation following femoral hemodialysis catheter exchange.
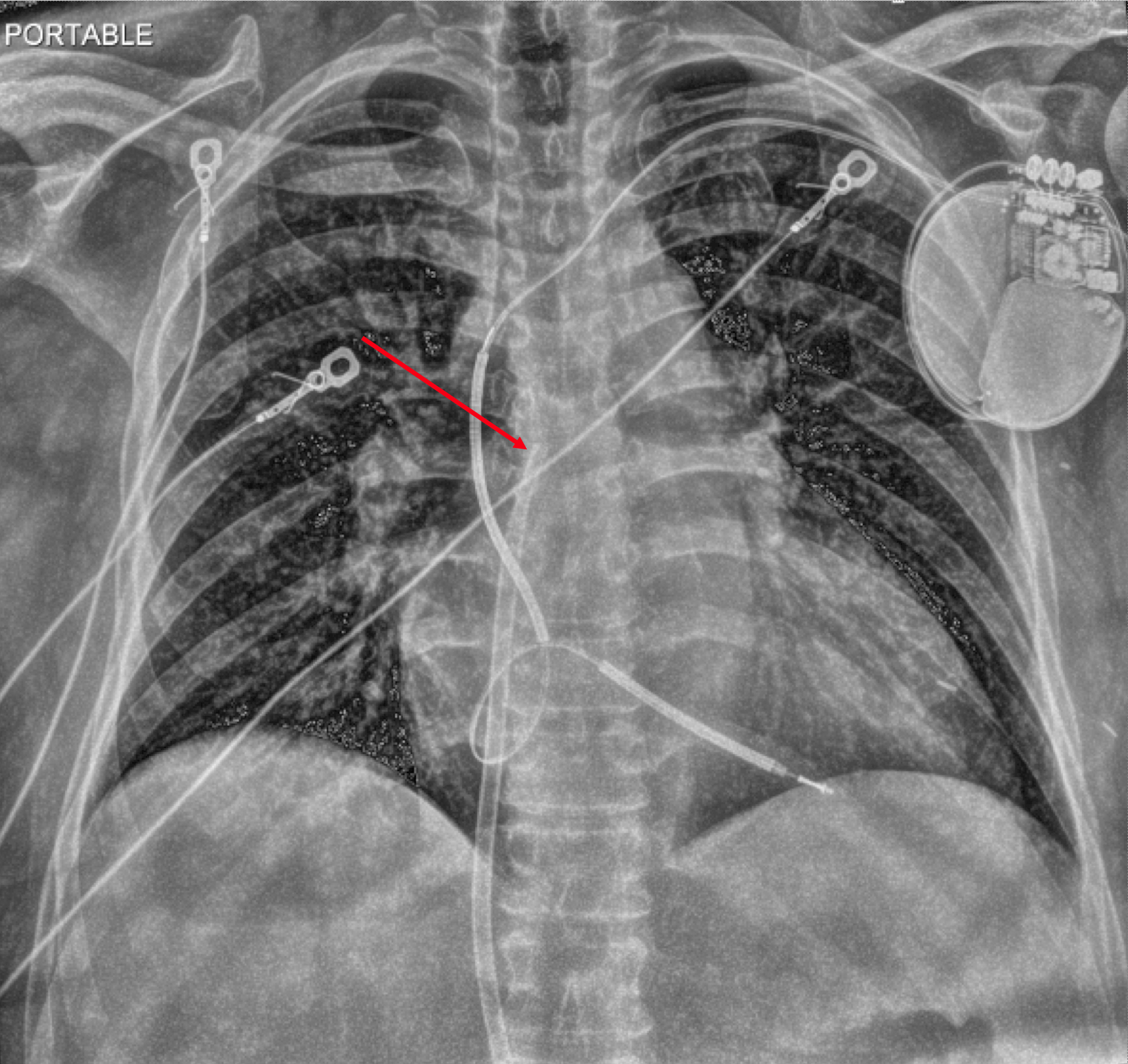
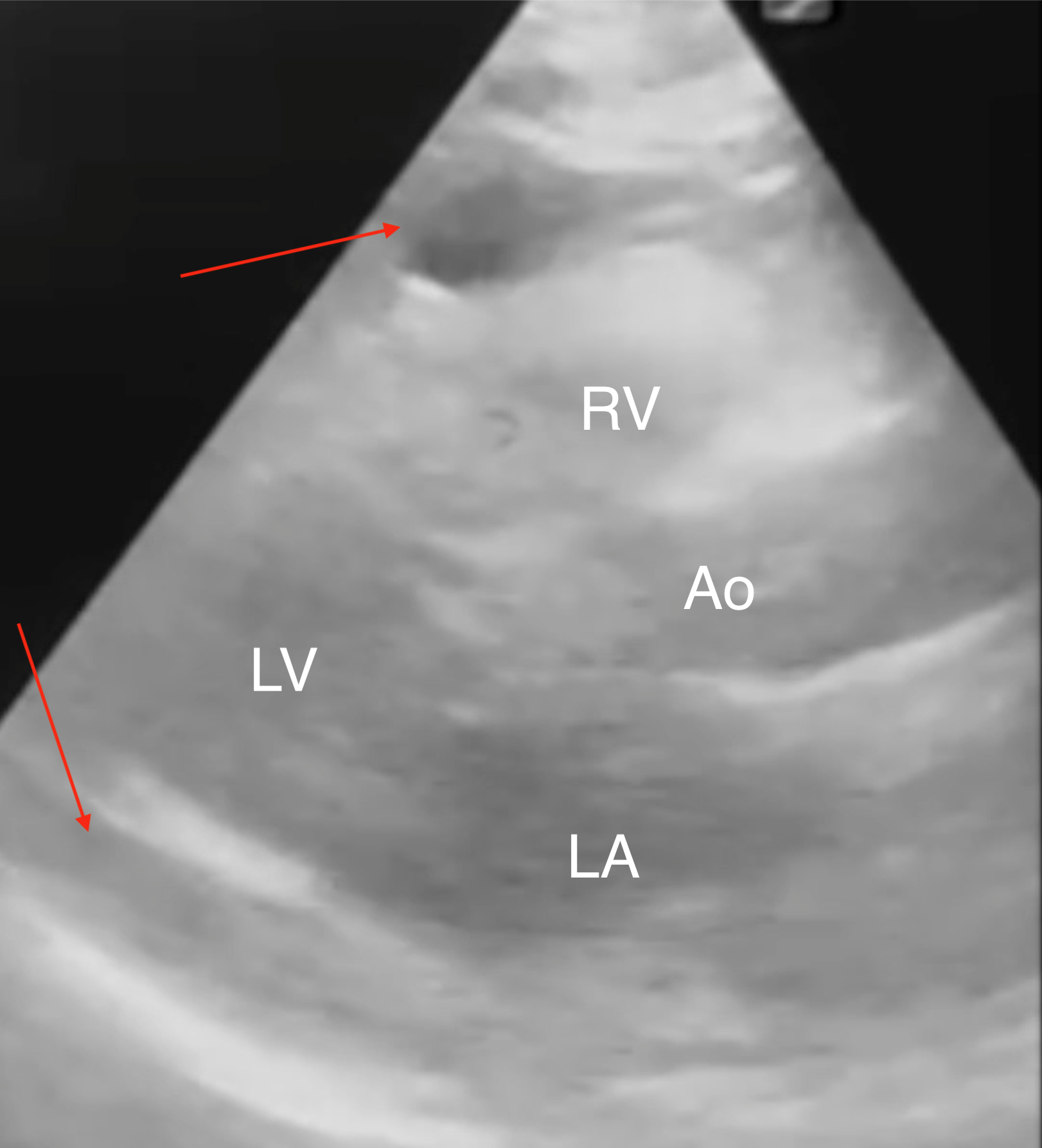
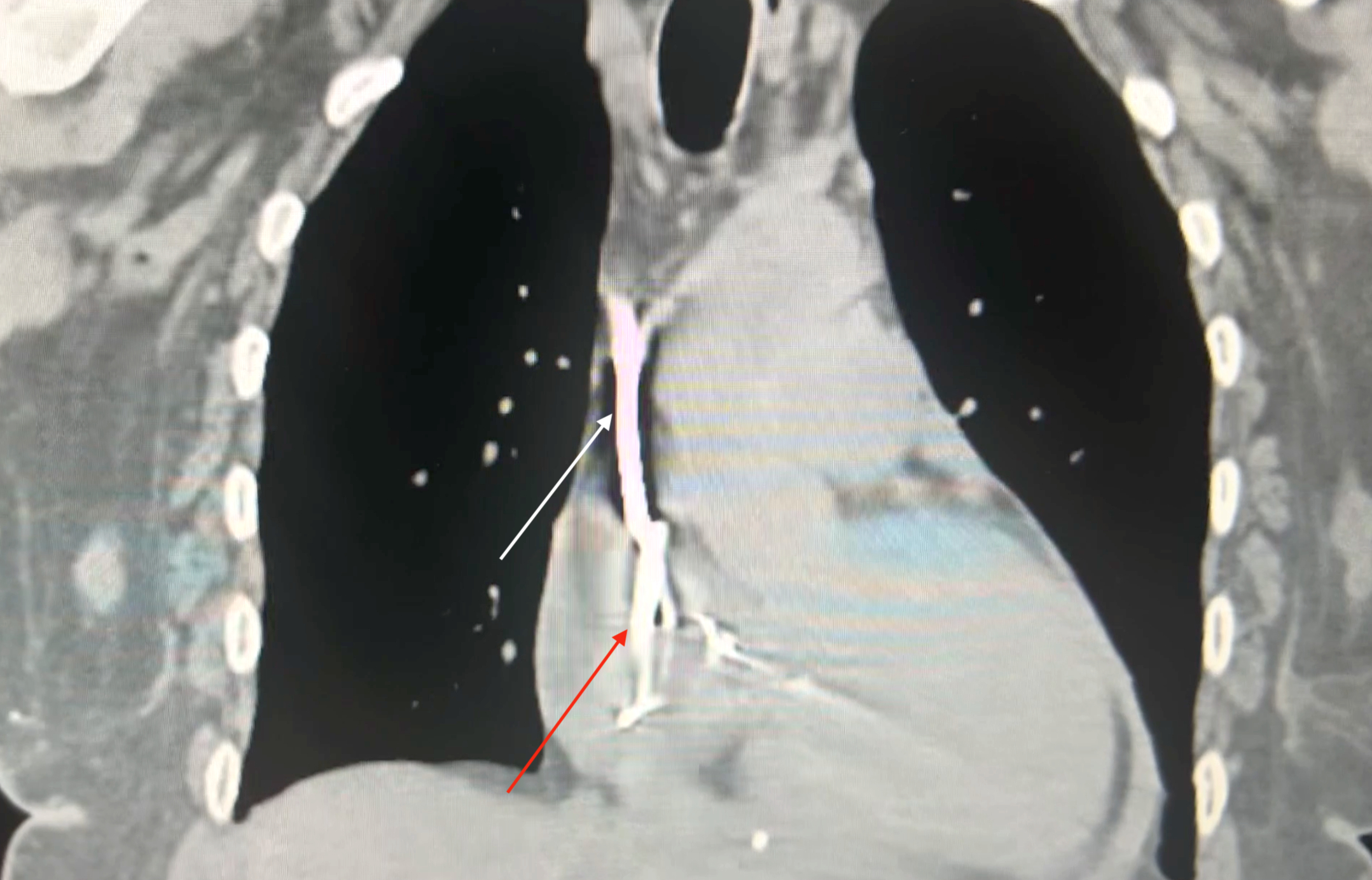
Case: A 61-year-old woman with heart failure with reduced ejection fraction (EF 25%), end-stage renal disease on hemodialysis, and a history of breast cancer presented with a malfunctioning hemodialysis catheter. After unsuccessful local alteplase, interventional radiology performed a left femoral hemodialysis catheter exchange. Within one hour post-procedure, the patient developed syncope, hypotension (60/40 mmHg), tachycardia (120 bpm), and reported chest discomfort, weakness, and lightheadedness. Bedside electrocardiogram showed sinus tachycardia with electrical alternans. Emergent echocardiography revealed a moderate circumferential pericardial effusion with right atrial systolic and right ventricular diastolic collapse, distended inferior vena cava, and marked respirophasic variation of atrioventricular inflow velocities, consistent with cardiac tamponade. Chest radiography suggested the catheter tip abutting the right atrial free wall. The delayed perforation was likely due to catheter migration and erosion. Despite aggressive fluid resuscitation and norepinephrine infusion (up to 35 mcg/hr), the patient remained unstable. Bedside pericardiocentesis drained approximately 700 mL of blood, resulting in rapid hemodynamic improvement and discontinuation of vasopressors within one hour. Computed tomography confirmed the catheter tip’s proximity to the right atrial wall. Cardiothoracic surgery determined that surgical intervention was unnecessary as the perforation had sealed spontaneously.
Conclusion: This case highlights the need for vigilance for mechanical complications, even with femoral central venous access. Immediate bedside echocardiography was critical for rapid diagnosis and intervention. The patient made a complete recovery following pericardiocentesis and was discharged asymptomatic on hospital day four.
Case: A 61-year-old woman with heart failure with reduced ejection fraction (EF 25%), end-stage renal disease on hemodialysis, and a history of breast cancer presented with a malfunctioning hemodialysis catheter. After unsuccessful local alteplase, interventional radiology performed a left femoral hemodialysis catheter exchange. Within one hour post-procedure, the patient developed syncope, hypotension (60/40 mmHg), tachycardia (120 bpm), and reported chest discomfort, weakness, and lightheadedness. Bedside electrocardiogram showed sinus tachycardia with electrical alternans. Emergent echocardiography revealed a moderate circumferential pericardial effusion with right atrial systolic and right ventricular diastolic collapse, distended inferior vena cava, and marked respirophasic variation of atrioventricular inflow velocities, consistent with cardiac tamponade. Chest radiography suggested the catheter tip abutting the right atrial free wall. The delayed perforation was likely due to catheter migration and erosion. Despite aggressive fluid resuscitation and norepinephrine infusion (up to 35 mcg/hr), the patient remained unstable. Bedside pericardiocentesis drained approximately 700 mL of blood, resulting in rapid hemodynamic improvement and discontinuation of vasopressors within one hour. Computed tomography confirmed the catheter tip’s proximity to the right atrial wall. Cardiothoracic surgery determined that surgical intervention was unnecessary as the perforation had sealed spontaneously.
Conclusion: This case highlights the need for vigilance for mechanical complications, even with femoral central venous access. Immediate bedside echocardiography was critical for rapid diagnosis and intervention. The patient made a complete recovery following pericardiocentesis and was discharged asymptomatic on hospital day four.
More abstracts on this topic:
A Diagnostic Pitfall: Subclavian Stenosis Mimicking Severe Aortic Stenosis on Echocardiography"
Ezaldin Shady, Abdelsalam Mahmoud, Elsayed Omar, Lee Marciano
Artificial Intelligence ECG Model To Reduce False-Positive STEMI Alerts in the Emergency DepartmentDavis Adam, Mesbah Heba, Boone Stephen