Final ID: MP1903
An Unusual Etiology of Tamponade: The Role of Solid Pericardial Debris
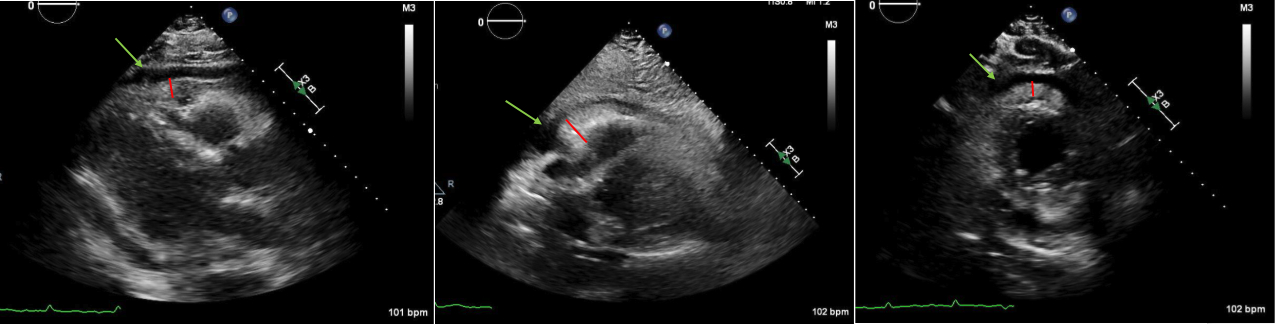
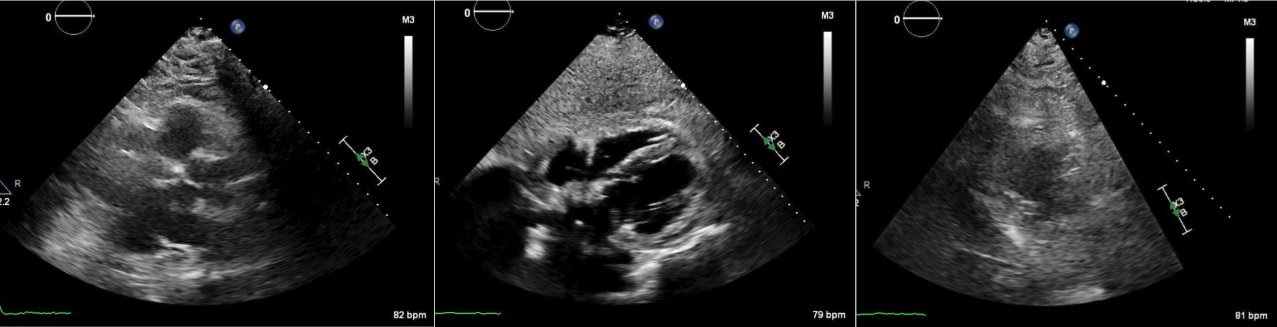
Abstract Body (Do not enter title and authors here): Case Description: A 71-year-old male presented to the hospital for dyspnea and chest discomfort for the past 2 weeks. He has a history of AAA status post stent and current tobacco use with emphysema. On admission, he was found to be tachycardic with rates reaching as high as 180 with systolic blood pressure of 89/61 and hypoxic with SpO2 of 80%. EKG revealed AFib with RVR with no acute ischemic changes. Troponins were negative and proBNP was 307. Infectious workup was negative. CTA chest showed no evidence of PE or dissection, however, moderate pericardial and bilateral pleural effusion was shown with mediastinal lymphadenopathy. After starting an esmolol and amiodarone drip, he converted to sinus tachycardia. TTE showed an EF 55%, echo dense debris measuring 2 cm with 1 cm effusion within the pericardial space resulting in significant compression of RA and RV. Findings were concerning for tamponade evidenced by invagination of RA and RV during systole and diastole respectively and greater than 50% variation and tricuspid inflow velocities with respiration. He was taken emergently to the OR for a pericardial window, thoracentesis, and chest tube. 300 mL and 400 mL of cloudy straw-colored fluid were removed from the pericardial and pleural space respectively. Fluid studies were negative for malignant cells and cultures remained negative. Repeat TTE showed an EF 55%, with epicardial fat pad and small posterior pericardial effusion. ANA testing was positive; however, other autoimmune studies are negative. His symptoms improved and he was discharged home.
Discussion: Cardiac tamponade is commonly caused by large pericardial effusions. Mild pericardial effusion less than 1 cm on TTE does not typically cause symptoms. However, the presence of significant pericardial debris can be problematic with minimal pericardial effusion. In this case, the patient developed cardiac tamponade complicated by AFib with RVR. Fortunately, hemodynamics and symptoms improved post pericardial window draining 300 mL of bloody fluid, but the diagnosis remains unknown given negative fluid studies. It's postulated that the debris is inflammatory in nature, but the absence of a diagnosis puts the patient at high risk for shock if the pericardial window fails. Patients with pericardial debris up to 2 cm on TTE with risk of developing pericardial effusion should be monitored with follow up TTE. Further studies are necessary to unveil the underlying etiology of large pericardial debris.
Discussion: Cardiac tamponade is commonly caused by large pericardial effusions. Mild pericardial effusion less than 1 cm on TTE does not typically cause symptoms. However, the presence of significant pericardial debris can be problematic with minimal pericardial effusion. In this case, the patient developed cardiac tamponade complicated by AFib with RVR. Fortunately, hemodynamics and symptoms improved post pericardial window draining 300 mL of bloody fluid, but the diagnosis remains unknown given negative fluid studies. It's postulated that the debris is inflammatory in nature, but the absence of a diagnosis puts the patient at high risk for shock if the pericardial window fails. Patients with pericardial debris up to 2 cm on TTE with risk of developing pericardial effusion should be monitored with follow up TTE. Further studies are necessary to unveil the underlying etiology of large pericardial debris.
More abstracts on this topic:
Comparative trends in decompressive hemicraniectomy in the era of mechanical thrombectomy among stroke patients (2016-2021) in the US National inpatient Sample.
Sohaib Muhammad, Maaz Hafiz, Chaychi Muhammad Tayyab Muzaffar, Rahman Haseeb, Saeed Daniaal, Kamal Haris, Ahmed Muhammad
A Bleeding Heart: Chronic Pericarditis Manifesting as Recurrent Hemorrhagic Pericardial Effusion - Diagnostic Considerations with a PFO Closure Device and the Role of CT ImagingPatel Zeel, Liu Yang, Wengrofsky Perry, Yoon Sung-han