Final ID: MP388
Redlining, Segregation, and Disparities in Heart Health: Structural Racism as a Driver of Adverse Cardiovascular Outcomes
Abstract Body (Do not enter title and authors here): Background:
Systemic barriers such as residential segregation and redlining exacerbate cardiovascular health disparities by restricting access to healthcare, socioeconomic opportunities, and environmental resources in racial and ethnic minority populations.
Objective:
To evaluate whether structural racism is associated with an increased risk of cardiovascular disease (CVD) in racial and ethnic minority populations compared to those with lower exposure to structural racism.
Methods:
A PRISMA-compliant systematic review and meta-analysis of observational studies published between 2000 and 2025 was conducted. Databases searched included PubMed, Embase, Web of Science, Scopus, and CINAHL. Eligible studies quantified structural racism using metrics such as segregation indices, redlining grades, or discrimination measures and reported cardiovascular outcomes in minority adults. Pooled analyses were performed using random-effects models. Eight studies (n ≈ 2.5 million participants) met inclusion criteria.
Results:
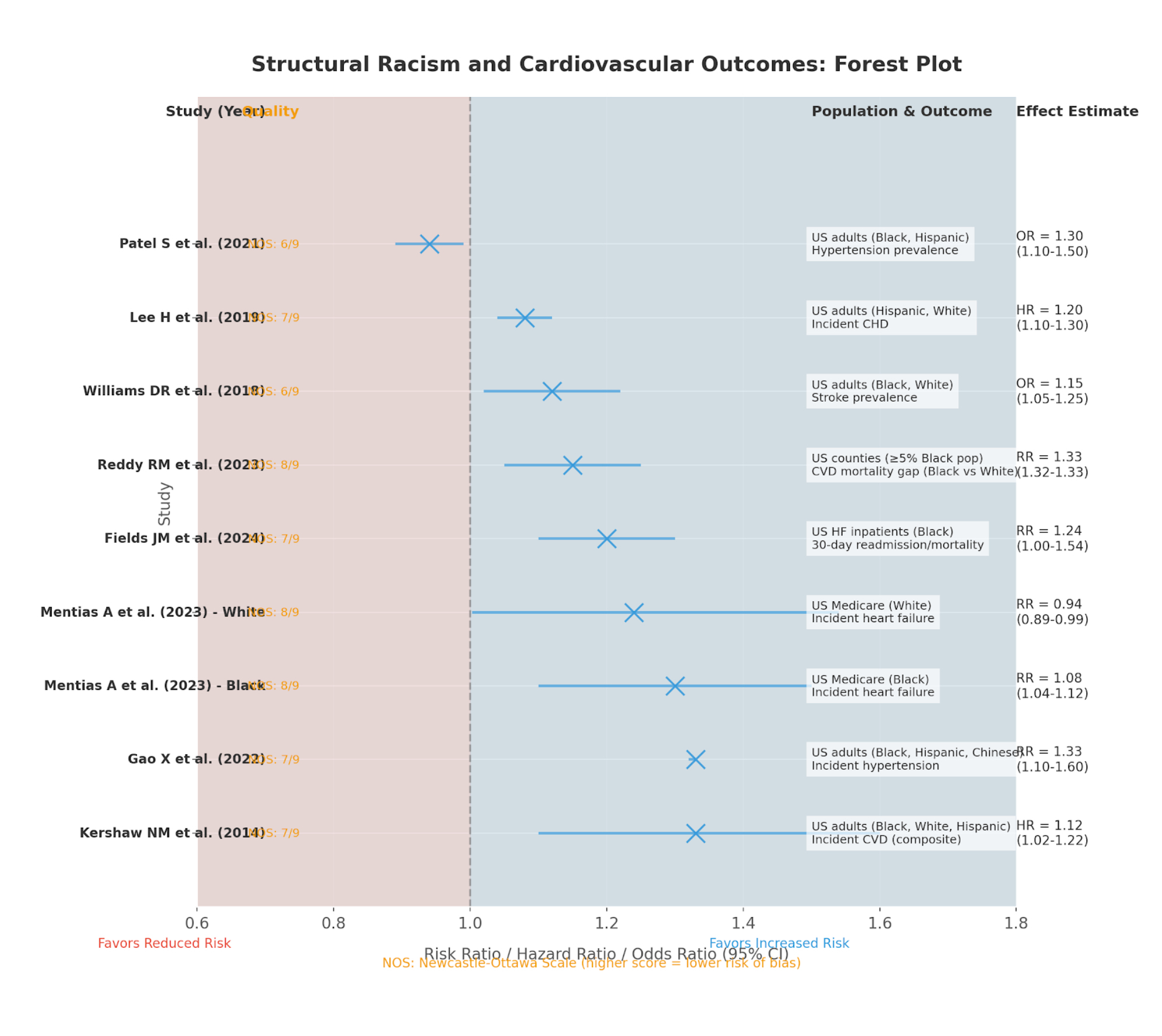
Structural racism indicators included neighborhood segregation (n = 3), historical redlining (n = 3), educational inequity (n = 1), and employment discrimination (n = 1). Outcomes assessed were incident CVD (n = 2), hypertension (n = 2), heart failure (n = 3), stroke (n = 1), and cardiovascular mortality gaps (n = 1). Study quality ranged from 6 to 8 (out of 9). Meta-analysis of five studies revealed a 21% increased risk of adverse cardiovascular outcomes with high structural racism exposure (pooled RR: 1.21; 95% CI: 1.05–1.39; Chi-square test = 98%). Specific findings included a 12% higher hazard for CVD per standard deviation increase in segregation among Black adults (HR: 1.12; 95% CI: 1.02–1.22), an 8% increased heart failure risk in historically redlined areas (RR: 1.08; 95% CI: 1.04–1.12), and a 33% greater Black–White mortality disparity in highly segregated counties (RR: 1.33; 95% CI: 1.32–1.33).
Conclusions:
Structural racism independently increases CVD risk in racial and ethnic minority populations, with segregation and redlining showing the strongest associations. These findings highlight the critical need for policy interventions to dismantle discriminatory systems, promote health equity, and reduce disparities in cardiovascular outcomes.
Systemic barriers such as residential segregation and redlining exacerbate cardiovascular health disparities by restricting access to healthcare, socioeconomic opportunities, and environmental resources in racial and ethnic minority populations.
Objective:
To evaluate whether structural racism is associated with an increased risk of cardiovascular disease (CVD) in racial and ethnic minority populations compared to those with lower exposure to structural racism.
Methods:
A PRISMA-compliant systematic review and meta-analysis of observational studies published between 2000 and 2025 was conducted. Databases searched included PubMed, Embase, Web of Science, Scopus, and CINAHL. Eligible studies quantified structural racism using metrics such as segregation indices, redlining grades, or discrimination measures and reported cardiovascular outcomes in minority adults. Pooled analyses were performed using random-effects models. Eight studies (n ≈ 2.5 million participants) met inclusion criteria.
Results:
Structural racism indicators included neighborhood segregation (n = 3), historical redlining (n = 3), educational inequity (n = 1), and employment discrimination (n = 1). Outcomes assessed were incident CVD (n = 2), hypertension (n = 2), heart failure (n = 3), stroke (n = 1), and cardiovascular mortality gaps (n = 1). Study quality ranged from 6 to 8 (out of 9). Meta-analysis of five studies revealed a 21% increased risk of adverse cardiovascular outcomes with high structural racism exposure (pooled RR: 1.21; 95% CI: 1.05–1.39; Chi-square test = 98%). Specific findings included a 12% higher hazard for CVD per standard deviation increase in segregation among Black adults (HR: 1.12; 95% CI: 1.02–1.22), an 8% increased heart failure risk in historically redlined areas (RR: 1.08; 95% CI: 1.04–1.12), and a 33% greater Black–White mortality disparity in highly segregated counties (RR: 1.33; 95% CI: 1.32–1.33).
Conclusions:
Structural racism independently increases CVD risk in racial and ethnic minority populations, with segregation and redlining showing the strongest associations. These findings highlight the critical need for policy interventions to dismantle discriminatory systems, promote health equity, and reduce disparities in cardiovascular outcomes.
More abstracts on this topic:
A Potential Role for NKG2D, an NK cell receptor, in Accelerated CVD risk in African American Women Living in More Adverse Neighborhood Conditions: Data From the Step It Up Physical Activity Digital Health-Enabled, Community-Engaged Intervention
Baez Andrew, Andrews Marcus, Sandler Dana, Aquino Peterson Elizabeth, Sharda Sonal, Tolentino Katherine Joy, Lopez De Leon Shirley, Seo Jein Eleanor, Cintron Manuel, Pita Mario, Tarfa Hannatu, Baumer Yvonne, Reger Robert, Childs Richard, Powell-wiley Tiffany, Dave Ayushi, Saurabh Abhinav, Mendelsohnl Laurel, Chen Long, Igboko Muna, Wells Ayanna, Marah Marie
Hypertensive Cardiorenal Disease with Cardiorenal Failure vs. Hypertensive Renal Disease with Renal Failure: Racial Mortality Trends from 1999 to 2020 in the United StatesAshfaq Fatima, Zain Ahmad