Final ID: MP414
Individual Social Determinants of Health, Area-Level Social Vulnerability and Incidence of Major Adverse Cardiovascular Events in a Primary Prevention Population: Real-World Evidence from The Houston Methodist CV Learning Health System (HM-CV-LHS) Registry
Abstract Body (Do not enter title and authors here): Introduction: Social determinants of health (SDOH) are key drivers of individual and population cardiovascular health. However, the relative effects of individual-level social determinants and neighborhood-level social vulnerability on new-onset major adverse cardiovascular events (MACE) have not been studied in a large primary prevention population in the US.
Methods: We conducted a retrospective cohort study of adults (≥18 years) without atherosclerotic cardiovascular disease (ASCVD) and available SDOH information in the 2016–2023 HM-CV-LHS dataset. Patient-level SDOH (medication affordability, food insecurity, transportation, depression) were assessed using the Epic SDOH wheel and aggregated to create a composite 3-level risk index (optimal, low, high). Neighborhood vulnerability was assessed using the CDC Social Vulnerability Index (SVI) and categorized into quartiles. Multivariable Cox proportional hazards models were used to assess the association between SDOH, SVI, and incident MACE. Harrell’s C-statistics were used to compare discriminant validity of individual SDOH, SVI and co-occurring SDOH/SVI models.
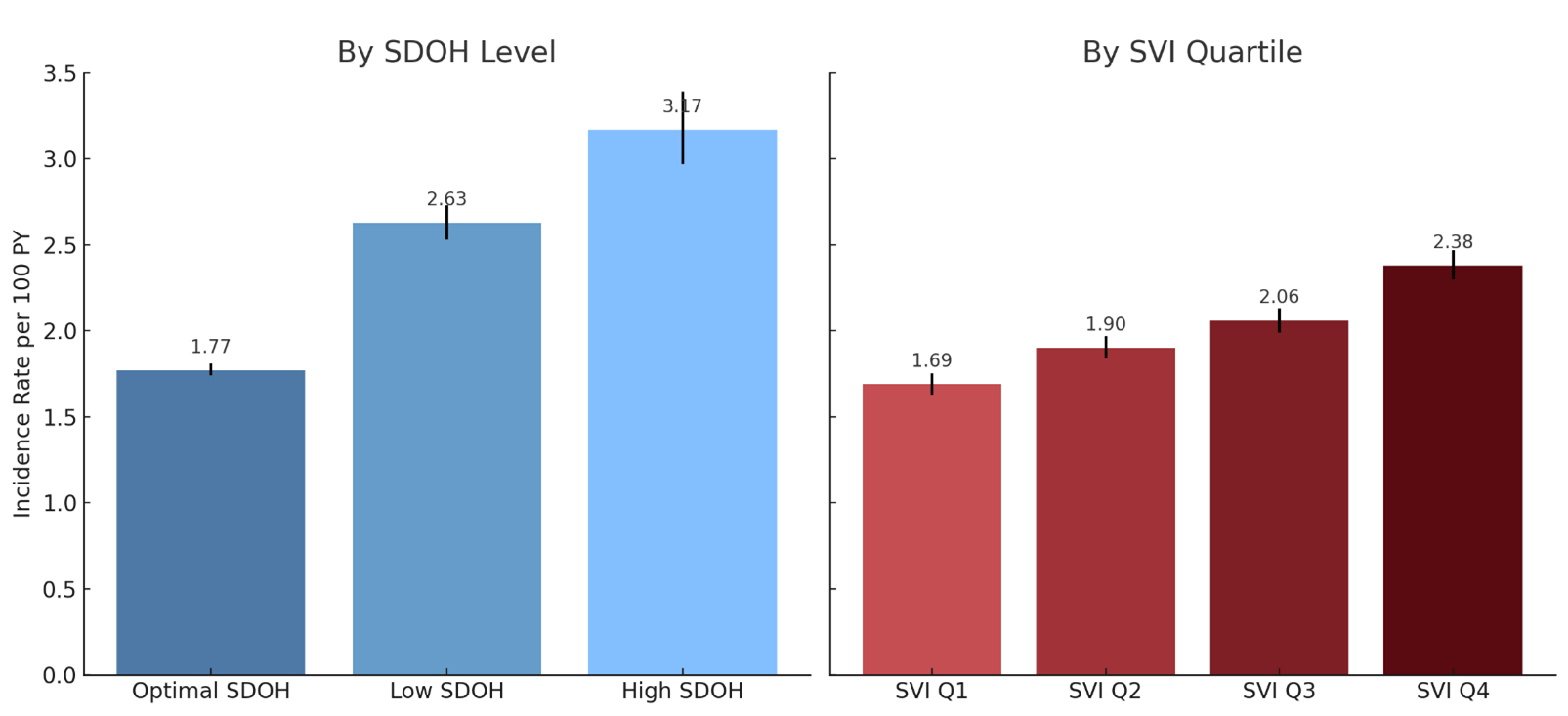
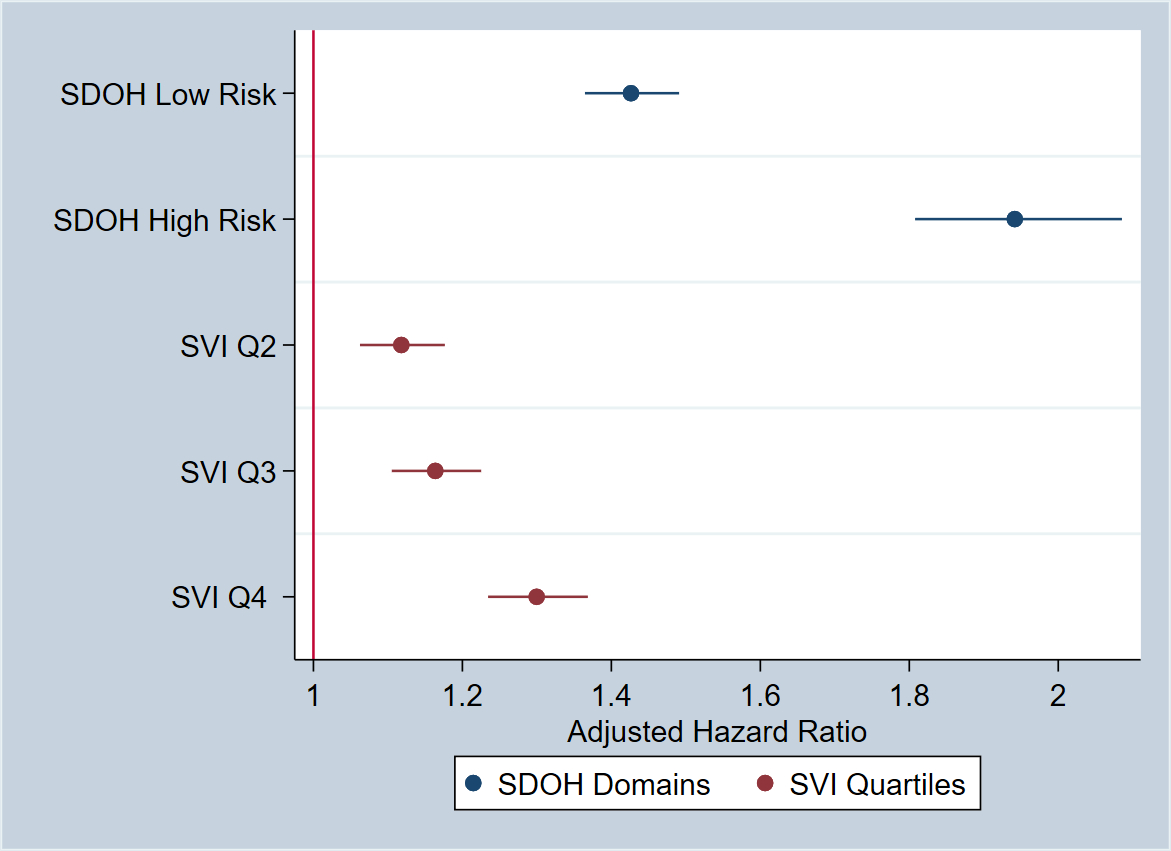
Results: Among 168,304 adults, 78% had optimal SDOH, 17% had low, and 5% had high SDOH burden. 8% lived in the least vulnerable (SVI-Q1) and 22% in the most vulnerable (Q4) neighborhoods. 12,268 MACE events were observed over 618,696 person-years follow-up. MACE incidence increased with higher SDOH and SVI burden (Figure 1). In fully adjusted models, individual-level SDOH burden had a relatively stronger effect on MACE risk (HR=1.94 [1.81–2.09] vs optimal SDOH) compared to neighborhood SVI burden (HR, Q4 vs Q1=1.30 [95% CI, 1.23–1.37]) (Figure 2), with the highest risk observed for combined SDOH/SVI model (HR=2.59 [95% CI, 2.30–2.92]). The models exhibited moderate discrimination: individual SDOH-only (C=0.727), SVI-only (C=0.722), co-occurring SDOH/SVI (C=0.729).
Conclusion: Both individual- and area-level social risk are independent predictors of MACE, and portend over 150% higher risk with co-occurring social burden. Efforts to address SDOH should target both patient and neighborhood level factors in order to mitigate MACE risk.
Methods: We conducted a retrospective cohort study of adults (≥18 years) without atherosclerotic cardiovascular disease (ASCVD) and available SDOH information in the 2016–2023 HM-CV-LHS dataset. Patient-level SDOH (medication affordability, food insecurity, transportation, depression) were assessed using the Epic SDOH wheel and aggregated to create a composite 3-level risk index (optimal, low, high). Neighborhood vulnerability was assessed using the CDC Social Vulnerability Index (SVI) and categorized into quartiles. Multivariable Cox proportional hazards models were used to assess the association between SDOH, SVI, and incident MACE. Harrell’s C-statistics were used to compare discriminant validity of individual SDOH, SVI and co-occurring SDOH/SVI models.
Results: Among 168,304 adults, 78% had optimal SDOH, 17% had low, and 5% had high SDOH burden. 8% lived in the least vulnerable (SVI-Q1) and 22% in the most vulnerable (Q4) neighborhoods. 12,268 MACE events were observed over 618,696 person-years follow-up. MACE incidence increased with higher SDOH and SVI burden (Figure 1). In fully adjusted models, individual-level SDOH burden had a relatively stronger effect on MACE risk (HR=1.94 [1.81–2.09] vs optimal SDOH) compared to neighborhood SVI burden (HR, Q4 vs Q1=1.30 [95% CI, 1.23–1.37]) (Figure 2), with the highest risk observed for combined SDOH/SVI model (HR=2.59 [95% CI, 2.30–2.92]). The models exhibited moderate discrimination: individual SDOH-only (C=0.727), SVI-only (C=0.722), co-occurring SDOH/SVI (C=0.729).
Conclusion: Both individual- and area-level social risk are independent predictors of MACE, and portend over 150% higher risk with co-occurring social burden. Efforts to address SDOH should target both patient and neighborhood level factors in order to mitigate MACE risk.
More abstracts on this topic:
12-lead electrocardiograms predict adverse cardiovascular outcomes of emergency department patients
Haimovich Julian, Kolossvary Marton, Alam Ridwan, Padros I Valls Raimon, Lu Michael, Aguirre Aaron
A Novel Missense Mutation in TNNT2 Gene in a Lebanese Pedigree With Ebstein Anomaly And Wolf-Parkinson-White Syndrome: A Case ReportAtasi Montaser, Dankar Razan, Barakat Salim, Wehbi Jad, Refaat Marwan