Final ID: MP29
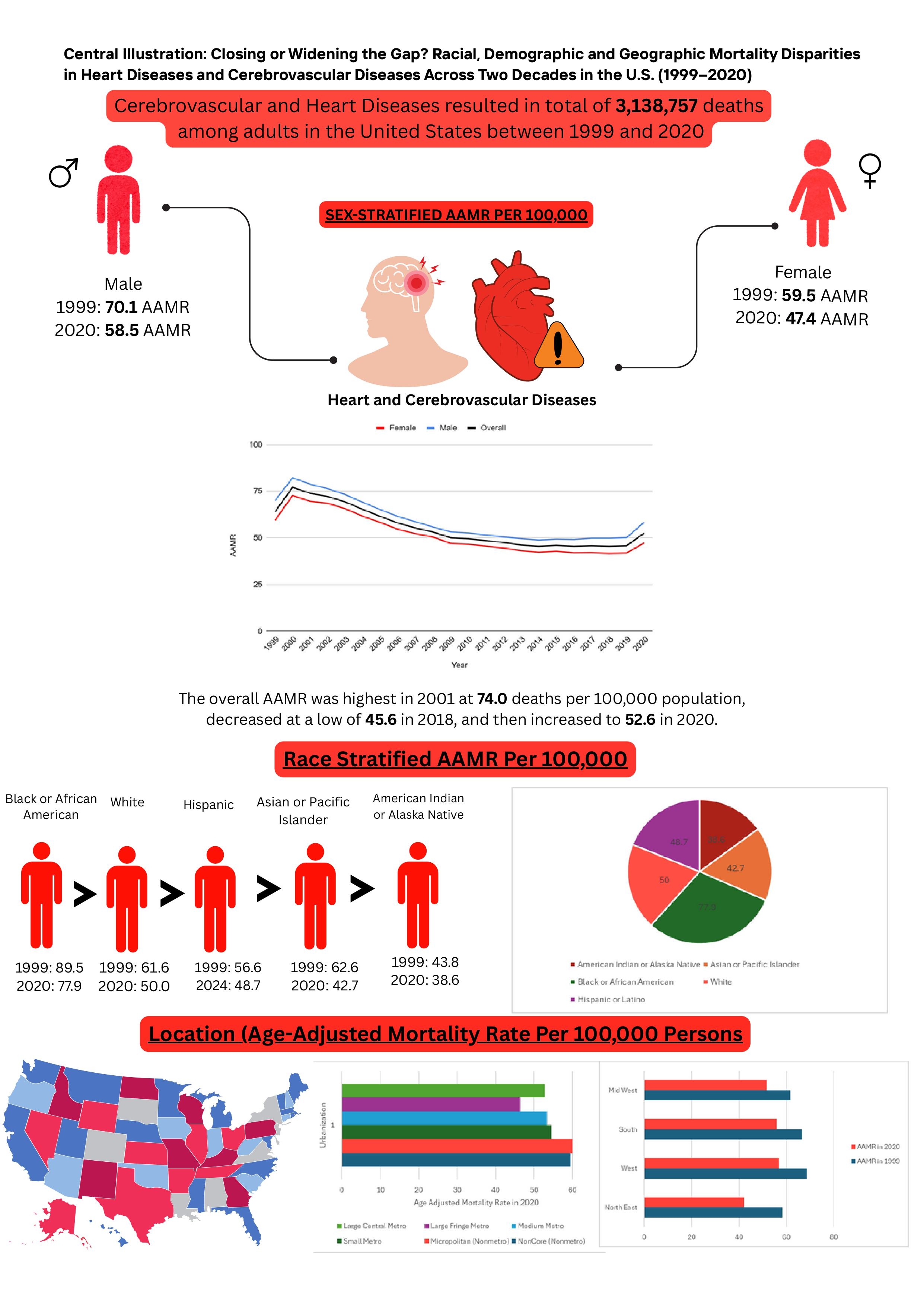
Closing or Widening the Gap? Racial, Demographic and Geographic Mortality Disparities in Heart Diseases and Cerebrovascular Diseases Across Two Decades in the U.S. (1999–2020)
Abstract Body (Do not enter title and authors here): Objective: This study aimed to analyze patterns in mortality related to heart and cerebrovascular diseases across different demographic groups and geographic regions in the adult population of United States.
Methods: Death certificates from the Centers for Disease Control and Prevention's Wide-Ranging Online Data for Epidemiologic Research database were examined to identify adults for whom heart and cerebrovascular diseases, ICD CODE: I00-I99 and I60-I69, were listed as either an underlying or contributing cause of death from 1999 to 2020. Age-adjusted mortality rates (AAMRs) per 100,000 individuals and annual percent changes (APC) were computed and categorized by year, sex, race/ethnicity, and geographic region (urban/rural and census region).
Results: From 1999 to 2020, there were 3,138,757 deaths associated with heart and cerebrovascular diseases among adults aged 15 years and older. The AAMR declined significantly from 64.1 in 1999 to 52.6 in 2020, with an overall average APC of –1.25 (95% CI: –1.6, –0.93; p<0.000001). Mortality rates initially rose between 1999 and 2001 (APC: 6.66; 95% CI: 0.97, 10.67; p=0.02), followed by a steady decline from 2001 to 2018, and a subsequent increase from 2018 to 2020 (APC: 7.98; 95% CI: 4.14, 10.77; p<0.000001). Women experienced a greater reduction in mortality (AAPC: –1.75; 95% CI: –2.19, –1.35; p<0.000001) compared to men (AAPC: –1.14; 95% CI: –1.48, –0.84; p<0.000001). Among racial and ethnic groups, Asian or Pacific Islanders had the greatest decline (AAPC: –2.25; 95% CI: –2.72, –1.77; p<0.000001). Regionally, the Northeast showed most marked decrease (AAPC: –1.91; 95% CI: –2.3, –1.59; p<0.000001), while large fringe metropolitan areas had the greatest decline among urban and rural classifications (AAPC: –1.54; 95% CI: –1.97, –1.13; p<0.000001). States in the top 90th percentile had approximately twice the AAMRs compared to those in the 10th percentile.
Conclusion: In conclusion, while overall AAMRs for heart and cerebrovascular diseases among U.S. adults have declined from 1999 to 2020, significant disparities remain across sex, race/ethnicity, geographic regions, and urbanization levels. The recent rise in mortality from 2018 to 2020 further underscores emerging public health concerns. Targeted interventions, including early identification, risk stratification, and tailored screening and management protocols in high-risk populations, are necessary to address and reduce mortality in light of these disparities.
Methods: Death certificates from the Centers for Disease Control and Prevention's Wide-Ranging Online Data for Epidemiologic Research database were examined to identify adults for whom heart and cerebrovascular diseases, ICD CODE: I00-I99 and I60-I69, were listed as either an underlying or contributing cause of death from 1999 to 2020. Age-adjusted mortality rates (AAMRs) per 100,000 individuals and annual percent changes (APC) were computed and categorized by year, sex, race/ethnicity, and geographic region (urban/rural and census region).
Results: From 1999 to 2020, there were 3,138,757 deaths associated with heart and cerebrovascular diseases among adults aged 15 years and older. The AAMR declined significantly from 64.1 in 1999 to 52.6 in 2020, with an overall average APC of –1.25 (95% CI: –1.6, –0.93; p<0.000001). Mortality rates initially rose between 1999 and 2001 (APC: 6.66; 95% CI: 0.97, 10.67; p=0.02), followed by a steady decline from 2001 to 2018, and a subsequent increase from 2018 to 2020 (APC: 7.98; 95% CI: 4.14, 10.77; p<0.000001). Women experienced a greater reduction in mortality (AAPC: –1.75; 95% CI: –2.19, –1.35; p<0.000001) compared to men (AAPC: –1.14; 95% CI: –1.48, –0.84; p<0.000001). Among racial and ethnic groups, Asian or Pacific Islanders had the greatest decline (AAPC: –2.25; 95% CI: –2.72, –1.77; p<0.000001). Regionally, the Northeast showed most marked decrease (AAPC: –1.91; 95% CI: –2.3, –1.59; p<0.000001), while large fringe metropolitan areas had the greatest decline among urban and rural classifications (AAPC: –1.54; 95% CI: –1.97, –1.13; p<0.000001). States in the top 90th percentile had approximately twice the AAMRs compared to those in the 10th percentile.
Conclusion: In conclusion, while overall AAMRs for heart and cerebrovascular diseases among U.S. adults have declined from 1999 to 2020, significant disparities remain across sex, race/ethnicity, geographic regions, and urbanization levels. The recent rise in mortality from 2018 to 2020 further underscores emerging public health concerns. Targeted interventions, including early identification, risk stratification, and tailored screening and management protocols in high-risk populations, are necessary to address and reduce mortality in light of these disparities.
More abstracts on this topic:
Assessing Veterans’ Risk of Cardiovascular Disease by Gender Identity
Streed Carl, Heier Kory, Oleary John, Jasuja Guneet, Goulet Joseph, Duncan Meredith
A Novel Animal Model for Pulmonary Hypertension: Lung Endothelial Specific Deletion of Egln1 in MiceLiu Bin, Yi Dan, Ramirez Karina, Fallon Michael, Dai Zhiyu