Final ID: Su3004
Left Bundle Branch Area Pacing versus Biventricular Pacing in Cardiac Resynchronization Therapy: An Updated Systematic Review and Meta-Analysis
Abstract Body (Do not enter title and authors here): Background:
Left bundle branch area pacing (LBB-P) has emerged as a physiologically targeted alternative to biventricular pacing (BiV-P) for cardiac resynchronization therapy (CRT). We conducted an updated systematic review and meta-analysis to compare the impact of LBBAP versus BiV-P on clinical and procedural outcomes in patients undergoing CRT.
Research Question:
Does left bundle branch area pacing (LBBAP) provide superior clinical and procedural outcomes compared to biventricular pacing (BiV-P) in patients receiving cardiac resynchronization therapy?
Methods:
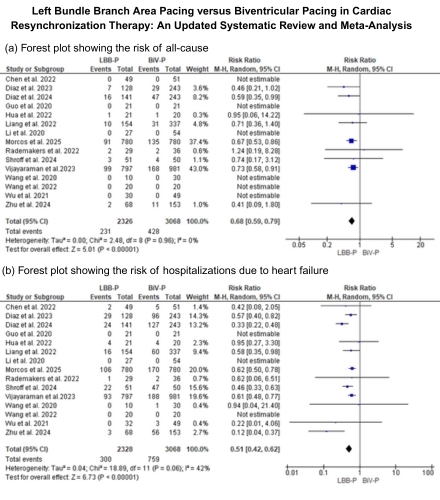
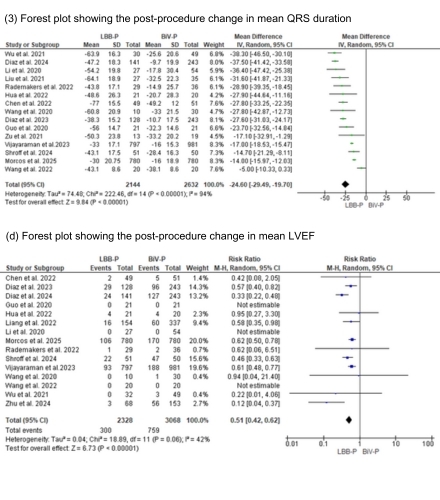
A systematic search of PubMed, Embase, and Cochrane Central was conducted in February 2025 to identify studies comparing LBB-P and BiV-P in patients undergoing CRT. Eligible studies included randomized and observational designs. Primary outcomes were all-cause mortality and heart failure–related hospitalization. Secondary outcomes included changes in QRS duration, Left ventricular ejection fraction (LVEF). Meta-analyses were performed using inverse-variance random-effects models. Heterogeneity was assessed using I2 and sensitivity was evaluated with leave-one-out analysis. Effect sizes were reported as relative risks (RR) or mean differences (MD) with corresponding 95% confidence intervals (CI).
Results:
Nineteen studies (18 observational and 1 randomized controlled trial) encompassing 5605 patients (LBB-P= 2428 and BiV-P= 3177) were included in this meta-analysis. Compared to BiV-P, LBB-P was associated with a significantly lower risk of all-cause mortality (RR = 0.68, 95% CI: 0.59–0.79; p < 0.00001) and HF-related hospitalization (RR = 0.51, 95% CI: 0.42–0.62; p < 0.00001). LBB-P was also associated with a greater narrowing of QRS duration (mean difference: –24.60 ms, 95% CI: –29.49 to –19.70; p < 0.00001) and greater improvement in LVEF (mean difference: 4.71%, 95% CI: 3.80 to 5.61; p < 0.0001).
Conclusion:
This updated meta-analysis demonstrates that LBB-P is associated with significantly lower all-cause mortality and HF-related hospitalizations compared to BiV-P in patients undergoing CRT. LBB-P also offers procedural advantages and greater improvements in electrical and functional cardiac parameters. Further large-scale randomized trials are warranted to confirm these findings.
Left bundle branch area pacing (LBB-P) has emerged as a physiologically targeted alternative to biventricular pacing (BiV-P) for cardiac resynchronization therapy (CRT). We conducted an updated systematic review and meta-analysis to compare the impact of LBBAP versus BiV-P on clinical and procedural outcomes in patients undergoing CRT.
Research Question:
Does left bundle branch area pacing (LBBAP) provide superior clinical and procedural outcomes compared to biventricular pacing (BiV-P) in patients receiving cardiac resynchronization therapy?
Methods:
A systematic search of PubMed, Embase, and Cochrane Central was conducted in February 2025 to identify studies comparing LBB-P and BiV-P in patients undergoing CRT. Eligible studies included randomized and observational designs. Primary outcomes were all-cause mortality and heart failure–related hospitalization. Secondary outcomes included changes in QRS duration, Left ventricular ejection fraction (LVEF). Meta-analyses were performed using inverse-variance random-effects models. Heterogeneity was assessed using I2 and sensitivity was evaluated with leave-one-out analysis. Effect sizes were reported as relative risks (RR) or mean differences (MD) with corresponding 95% confidence intervals (CI).
Results:
Nineteen studies (18 observational and 1 randomized controlled trial) encompassing 5605 patients (LBB-P= 2428 and BiV-P= 3177) were included in this meta-analysis. Compared to BiV-P, LBB-P was associated with a significantly lower risk of all-cause mortality (RR = 0.68, 95% CI: 0.59–0.79; p < 0.00001) and HF-related hospitalization (RR = 0.51, 95% CI: 0.42–0.62; p < 0.00001). LBB-P was also associated with a greater narrowing of QRS duration (mean difference: –24.60 ms, 95% CI: –29.49 to –19.70; p < 0.00001) and greater improvement in LVEF (mean difference: 4.71%, 95% CI: 3.80 to 5.61; p < 0.0001).
Conclusion:
This updated meta-analysis demonstrates that LBB-P is associated with significantly lower all-cause mortality and HF-related hospitalizations compared to BiV-P in patients undergoing CRT. LBB-P also offers procedural advantages and greater improvements in electrical and functional cardiac parameters. Further large-scale randomized trials are warranted to confirm these findings.
More abstracts on this topic:
Clinical Outcomes of Conduction System Pacing Versus Right Ventricular Pacing: A Systematic Review and Meta-Analysis of Initial Pacemaker Implantation
Fernandes Oliveira Amador Wellgner, Queiroga Flavia, Arrighini Giang Son, Odozynski Gabriel, Iqbal Asad, Oliveira Fonseca Pandora Eloa, Bisneto Oscar, Itaya Eduardo Dan, Oliveira Carneiro Alexandre, Giorgi Juliana, Assis Theodora, Cruz Akabane Maria Antonia
Device Dislodgement and Embolization associated with a New Leadless PacemakerBahbah Ali, Sengupta Jay, Witt Dawn, Zishiri Edwin, Zakaib John, Abdelhadi Raed, Hauser Robert