Final ID: Su4099
Catheter-Directed Intervention for High-Risk Acute Pulmonary Embolism in Chronic Kidney Disease
Abstract Body (Do not enter title and authors here): Background: Catheter-Directed Interventions (CDIs) for Acute Pulmonary Embolism (PE) have been present for years but their use is limited due to paucity of data especially in patients with chronic kidney disease (CKD). We aim to compare safety and efficacy of CDIs in CKD patients with high-risk PE.
Methods: Nationwide Readmissions Database (2016-2021) was used to identify CKD patients presenting with high-risk PE (HR-PE) (shock, pressor or mechanical circulatory support requirement). We included CKD stages 3 and above including end-stage kidney disease (ESKD). Patients who received systematic thrombolysis were excluded. Mahalanobis Distance Matching within the Propensity Score Caliper was used to match patient who received CDIs vs those who did not. Inverse Probability weighting (IPW) was utilized, and Pearson’s chi-squared test was applied to the PSM-2 matched cohorts to compare outcomes.
Results: Among 931,585 hospitalizations of CKD patients with HR-PE, 1,404 (0.2%) of the patients underwent CDI.
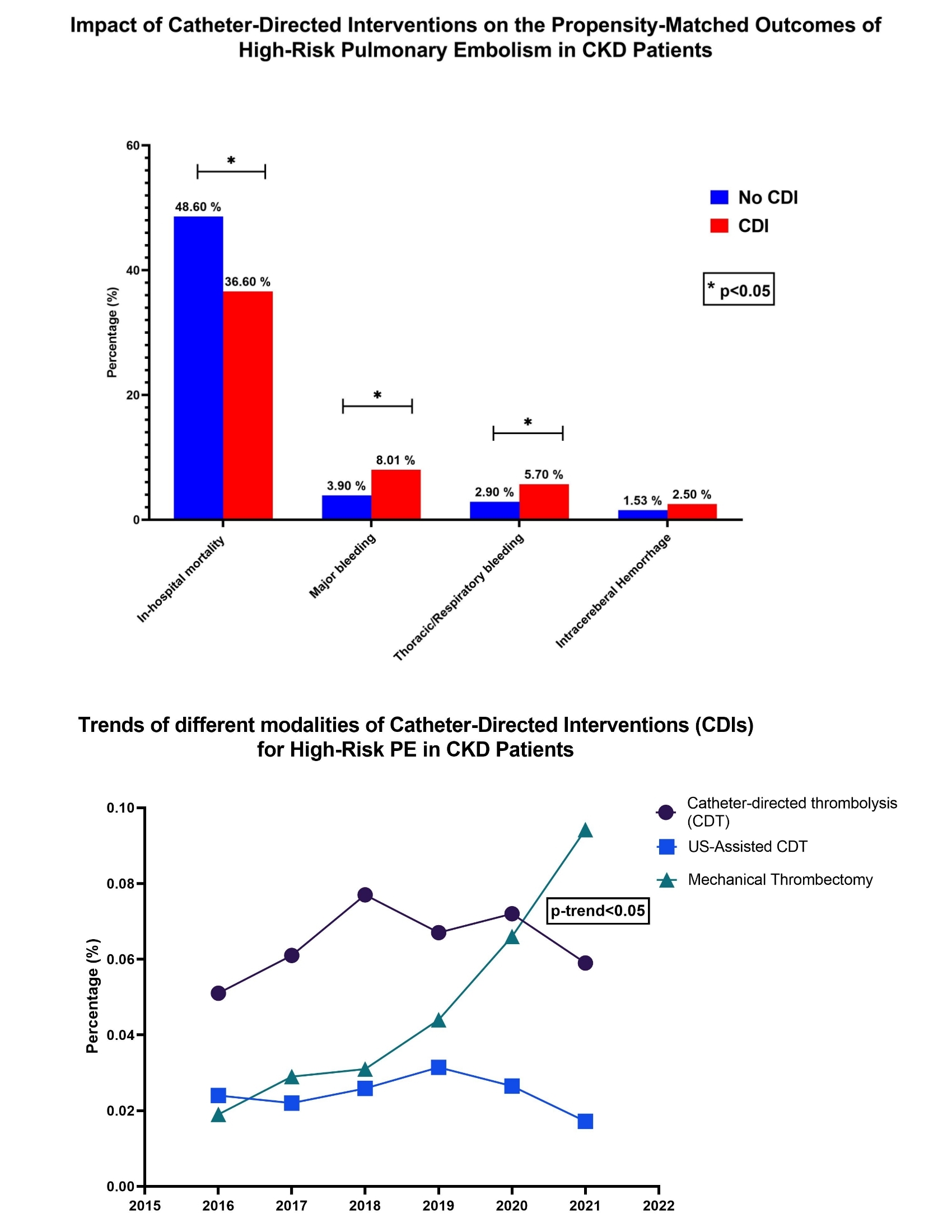
After propensity matching (N: 718 in each group), patients receiving CDI had a significantly lower mortality (36.6% vs. 48.6%, aOR:0.61, p <0.001). However, bleeding complications including major bleeding (8.1% vs 3.9%, aOR:1.7, p: 0.001), thoraco-respiratory bleeding (5.7% vs 2.9%, aOR:1.6, p <0.001) was higher in patients receiving CDIs. No difference was observed the risk of intracerebral hemorrhage (p>0.05). Readmission rates were similar at 30-day, 90-day and 180-day intervals (p>0.05). From 2016-2021, mortality associated with HR-PE in CKD patients has slightly increased (49.1% to 49.5%, p: 0.024). There has been increasing use of mechanical thrombectomy (MT) over thrombolysis in recent years (0.02% to 0.09%, p-trend <0.01).
Conclusion: CDIs for HR-PE in CKD patients are associated with significant reduction in mortality at an expense of higher bleeding risk. Despite slight increase in the utilization of MT, mortality has not significantly decreased across the years.
Methods: Nationwide Readmissions Database (2016-2021) was used to identify CKD patients presenting with high-risk PE (HR-PE) (shock, pressor or mechanical circulatory support requirement). We included CKD stages 3 and above including end-stage kidney disease (ESKD). Patients who received systematic thrombolysis were excluded. Mahalanobis Distance Matching within the Propensity Score Caliper was used to match patient who received CDIs vs those who did not. Inverse Probability weighting (IPW) was utilized, and Pearson’s chi-squared test was applied to the PSM-2 matched cohorts to compare outcomes.
Results: Among 931,585 hospitalizations of CKD patients with HR-PE, 1,404 (0.2%) of the patients underwent CDI.
After propensity matching (N: 718 in each group), patients receiving CDI had a significantly lower mortality (36.6% vs. 48.6%, aOR:0.61, p <0.001). However, bleeding complications including major bleeding (8.1% vs 3.9%, aOR:1.7, p: 0.001), thoraco-respiratory bleeding (5.7% vs 2.9%, aOR:1.6, p <0.001) was higher in patients receiving CDIs. No difference was observed the risk of intracerebral hemorrhage (p>0.05). Readmission rates were similar at 30-day, 90-day and 180-day intervals (p>0.05). From 2016-2021, mortality associated with HR-PE in CKD patients has slightly increased (49.1% to 49.5%, p: 0.024). There has been increasing use of mechanical thrombectomy (MT) over thrombolysis in recent years (0.02% to 0.09%, p-trend <0.01).
Conclusion: CDIs for HR-PE in CKD patients are associated with significant reduction in mortality at an expense of higher bleeding risk. Despite slight increase in the utilization of MT, mortality has not significantly decreased across the years.
More abstracts on this topic:
Association between Pulmonary Artery Elastance and all cause mortality in patients with Heart Failure: A Meta-Analysis
Mellacheruvu Sai Priyanka, Rizvi Bisharah, Nagarajan Jai Sivanandan, Vasudevan Srivatsa Surya, Pingili Adhvithi, Mohnani Priyanka, Kaur Shreyjit, Adompreh-fia Kokou, Sivakumar Thiruvikram, Pendem Harini
A Cross-scale Causal Machine Learning Framework Pinpoints Mgl2+ Macrophage Orchestrators of Balanced Arterial GrowthHan Jonghyeuk, Kong Dasom, Schwarz Erica, Takaesu Felipe, Humphrey Jay, Park Hyun-ji, Davis Michael E