Final ID: MP59
Vital Signs of Survival: Do Trends in Mixed Venous Oxygen Saturation and Lactic Acidosis Predict ICU Mortality?
Abstract Body (Do not enter title and authors here): Background:
Mixed venous oxygen saturation (SVO2), a direct marker of circulatory adequacy measured in the pulmonary artery, has been proposed as a more immediate reflection of perfusion compared to serum lactate, which can be delayed due to clearance variability and lab turnaround. While central venous oxygen saturation (ScVO2) is commonly used in shock management, data on the prognostic value of SVO2 remains inconsistent. This study evaluates whether trends in SVO2 and lactic acid over 72 hours are associated with ICU mortality, and whether monitoring SVO2 offers clinical benefit.
Methods:
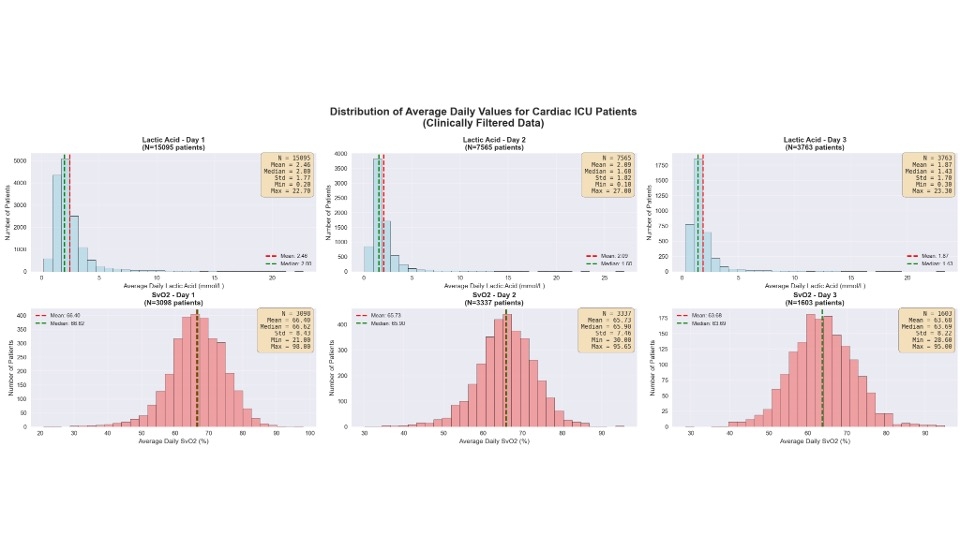
From the MIMIC-IV ICU database (n=34,222), 3,149 patients with SVO2 measurements were included. Patients were stratified into four groups based on SVO2 and lactate trends from ICU admission to 72 hours:
SVO2 Groups :
BB: Below–Below: SVO2 <55% at both timepoints (q1: 51%, q3: 60%)
BA: Below–Above: SVO2 <55% initially, improved to >65% (q1: 58%, q3: 68%)
AA: Above–Above: SVO2 ≥65% consistently (q1: 72%, q3: 79%)
AB: Above–Below: SVO2 >65% initially, dropped to <55% (q1: 62%, q3: 72%)
Lactic Acid Groups:
BB: Below–Below: <2 mmol/L throughout (q1: 1, q3: 1.6)
BA: Below–Above: <2 initially, rose to >2 (q1: 1.5, q3: 2.8)
AA: Above–Above: >2 consistently (q1: 2.6, q3: 5.4)
AB: Above–Below: >2 initially, fell to <2 (q1: 1.6, q3: 2.9)
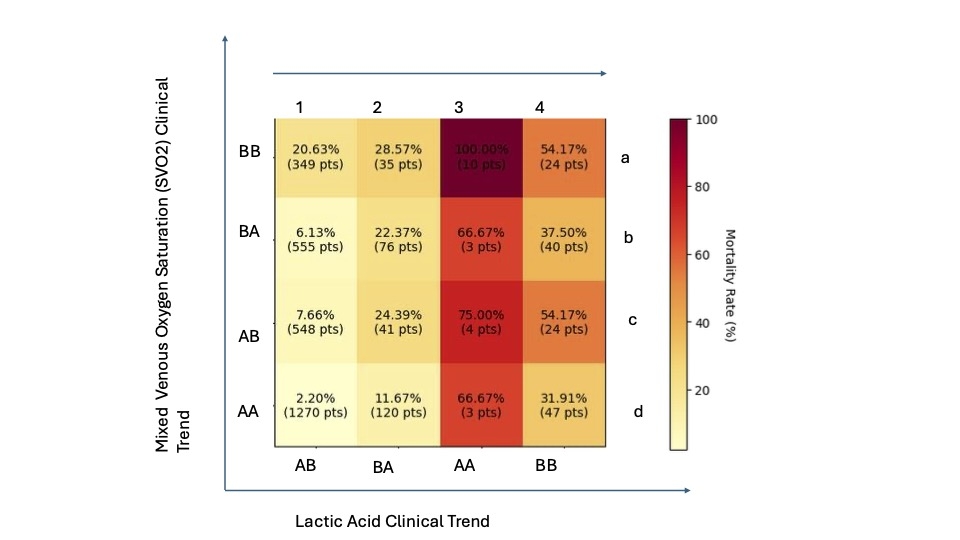
We then constructed a heat map to compare %mortality at 30 days in these groups.
Results:
The highest mortality (100%) occurred in patients with persistently elevated lactate (>2 mmol/L) and low SVO2 (<55%) (group 3a). The second-highest mortality (75%) was observed in those with persistently elevated lactate but improved SVO2(3c). Notably, among patients with improved lactate, mortality was similar regardless of whether SVO2 improved or remained low ($a vs 4c). This suggests that lactic acid trends may be a more reliable prognostic marker than SVO2.
Conclusion:
Improvement in SVO2 over 72 hours does not necessarily correlate with improved ICU survival. Persistent hyperlactatemia remains a stronger predictor of mortality. These findings question the clinical utility and cost-effectiveness of routine SVO2 monitoring in ICU settings.
Mixed venous oxygen saturation (SVO2), a direct marker of circulatory adequacy measured in the pulmonary artery, has been proposed as a more immediate reflection of perfusion compared to serum lactate, which can be delayed due to clearance variability and lab turnaround. While central venous oxygen saturation (ScVO2) is commonly used in shock management, data on the prognostic value of SVO2 remains inconsistent. This study evaluates whether trends in SVO2 and lactic acid over 72 hours are associated with ICU mortality, and whether monitoring SVO2 offers clinical benefit.
Methods:
From the MIMIC-IV ICU database (n=34,222), 3,149 patients with SVO2 measurements were included. Patients were stratified into four groups based on SVO2 and lactate trends from ICU admission to 72 hours:
SVO2 Groups :
BB: Below–Below: SVO2 <55% at both timepoints (q1: 51%, q3: 60%)
BA: Below–Above: SVO2 <55% initially, improved to >65% (q1: 58%, q3: 68%)
AA: Above–Above: SVO2 ≥65% consistently (q1: 72%, q3: 79%)
AB: Above–Below: SVO2 >65% initially, dropped to <55% (q1: 62%, q3: 72%)
Lactic Acid Groups:
BB: Below–Below: <2 mmol/L throughout (q1: 1, q3: 1.6)
BA: Below–Above: <2 initially, rose to >2 (q1: 1.5, q3: 2.8)
AA: Above–Above: >2 consistently (q1: 2.6, q3: 5.4)
AB: Above–Below: >2 initially, fell to <2 (q1: 1.6, q3: 2.9)
We then constructed a heat map to compare %mortality at 30 days in these groups.
Results:
The highest mortality (100%) occurred in patients with persistently elevated lactate (>2 mmol/L) and low SVO2 (<55%) (group 3a). The second-highest mortality (75%) was observed in those with persistently elevated lactate but improved SVO2(3c). Notably, among patients with improved lactate, mortality was similar regardless of whether SVO2 improved or remained low ($a vs 4c). This suggests that lactic acid trends may be a more reliable prognostic marker than SVO2.
Conclusion:
Improvement in SVO2 over 72 hours does not necessarily correlate with improved ICU survival. Persistent hyperlactatemia remains a stronger predictor of mortality. These findings question the clinical utility and cost-effectiveness of routine SVO2 monitoring in ICU settings.
More abstracts on this topic:
The Impact of a Closed Unit Model on Cardiac Intensive Care Unit Outcomes: A Before-After Study
Hinkamp Colin, Nardi Matthew, Senussi Mourad
Ambulatory Breath Analyzer for Measuring Cardiac OutputHale Joshua, Kolomenski Alexandre, Schuessler Hans, Tong Carl