Final ID: MP56
25-Year Decline in Aortic Aneurysm and Dissection Mortality in the U.S.: Impact of Endovascular Repair and Forecast to 2030
Abstract Body (Do not enter title and authors here):
Introduction: Aortic aneurysm and dissection are rare but life-threatening conditions, with an incidence of 5–30 cases per million annually. The introduction of endovascular aneurysm repair (EVAR) has markedly improved outcomes. This study analyzes 25-year U.S. mortality trends (1999–2023) and forecasts rates through 2030.
Methodology: We analyzed national mortality data from the CDC WONDER database (1999–2023) using ICD-10 codes I71.0–I71.9 to identify deaths due to aortic aneurysm and dissection. Age-adjusted mortality rates (AAMRs) were stratified by demographics and geography, based on NCHS urban–rural and U.S. Census regional classifications. Trends were assessed using Joinpoint regression to estimate Annual and Average Annual Percentage Changes (APC/AAPC) with 95% confidence intervals. ARIMA models with Box-Cox transformation were fitted after ADF/KPSS tests
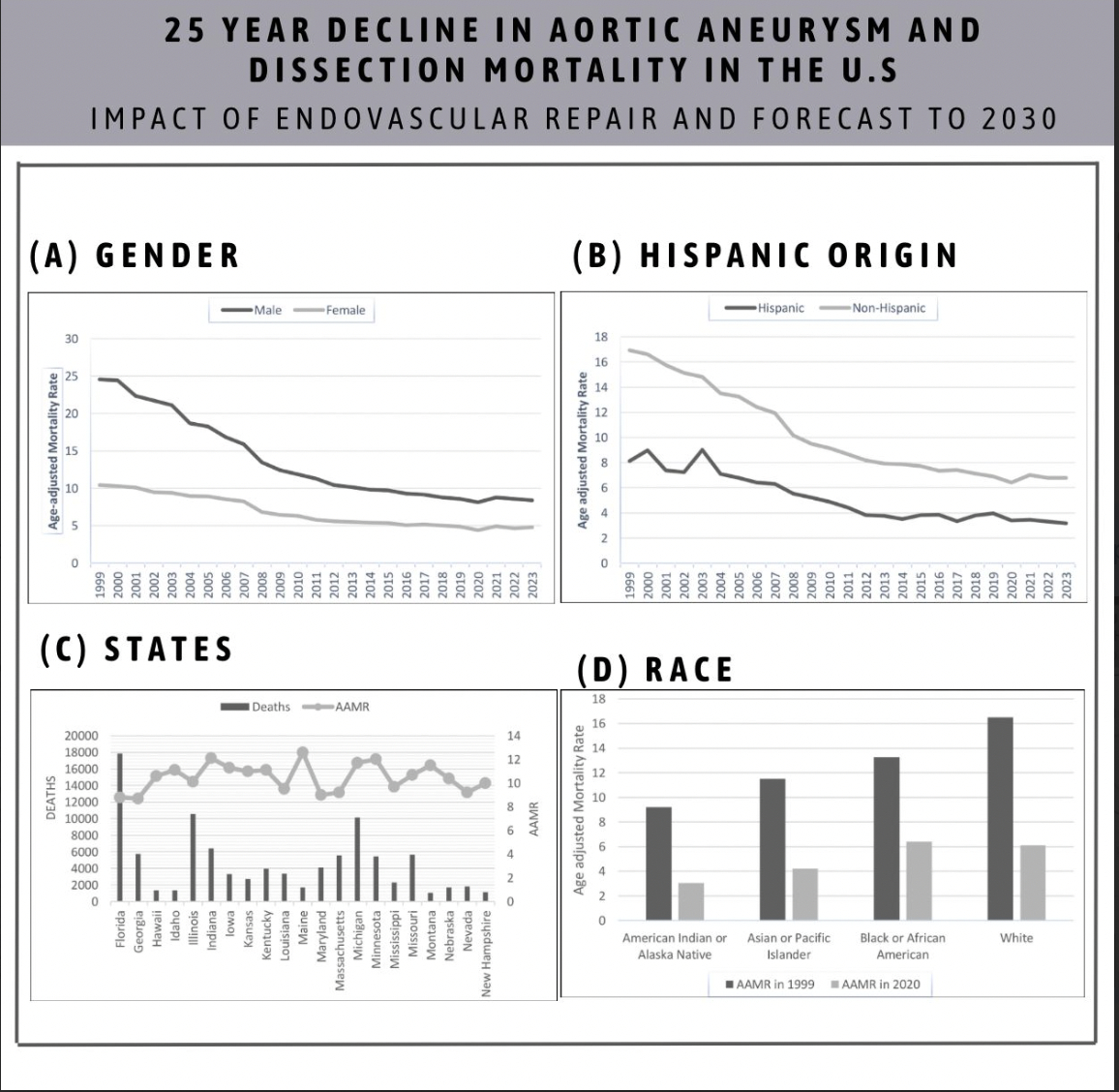
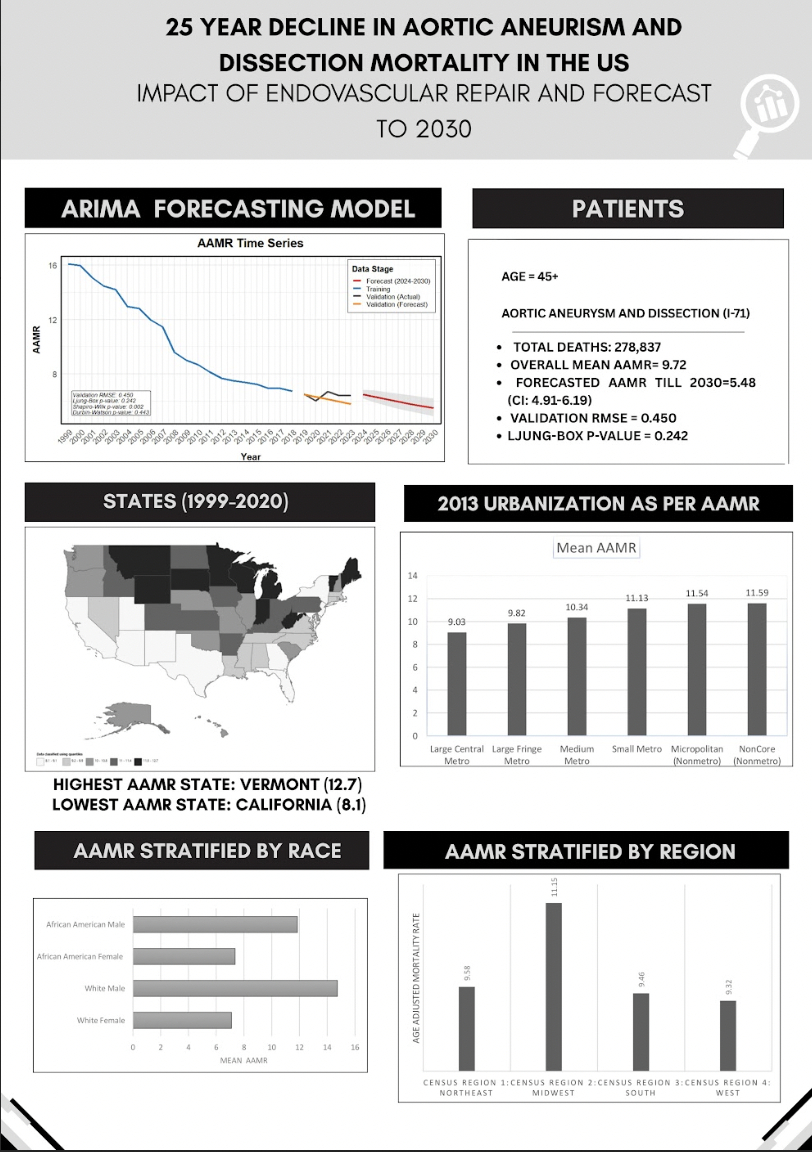
Results: From 1999 to 2023, the age-adjusted mortality rate (AAMR) for aortic aneurysm and dissection in the U.S. declined markedly from 15.88 to 6.6 per 100,000. ARIMA modeling forecasted an AAMR of 6.32 (95% CI: 5.90–6.79) in 2025 and 5.48 (95% CI: 4.92–6.19) in 2030, with good model fit (RMSE = 0.450; Ljung-Box p = 0.242). Joinpoint regression identified the most rapid decline between 2006 and 2009 (Annual Percent Change [APC] = –10.78), coinciding with the widespread adoption of endovascular aneurysm repair (EVAR), despite its initially delayed adoption into clinical practice. Urban–rural disparities were evident, with the most significant decline observed in large central metro areas (AAMR: 14.52 to 5.16) compared to non-core rural areas (18.25 to 7.38). Regionally, the Midwest had the highest mortality in 1999 and experienced the steepest decline over time. Racial disparities persisted, with White individuals accounting for the highest number of deaths but also demonstrating the most pronounced decline (AAMR: 16.5 to 6.12; APC = –5.35). Non-Hispanic males had the highest mortality rates overall (AAMR: 24.55 to 8.39; AAPC = –4.61), while Hispanic females consistently had the lowest.
Conclusions: From 1999 to 2023, mortality from aortic aneurysm and dissection declined significantly, driven by advances such as endovascular aneurysm repair (EVAR) and improved clinical care. However, notable disparities by race, sex, and region remain despite these advances, highlighting the need for patient-centered selection, ongoing outcome reevaluation, and an equitable approach to care delivery.
Introduction: Aortic aneurysm and dissection are rare but life-threatening conditions, with an incidence of 5–30 cases per million annually. The introduction of endovascular aneurysm repair (EVAR) has markedly improved outcomes. This study analyzes 25-year U.S. mortality trends (1999–2023) and forecasts rates through 2030.
Methodology: We analyzed national mortality data from the CDC WONDER database (1999–2023) using ICD-10 codes I71.0–I71.9 to identify deaths due to aortic aneurysm and dissection. Age-adjusted mortality rates (AAMRs) were stratified by demographics and geography, based on NCHS urban–rural and U.S. Census regional classifications. Trends were assessed using Joinpoint regression to estimate Annual and Average Annual Percentage Changes (APC/AAPC) with 95% confidence intervals. ARIMA models with Box-Cox transformation were fitted after ADF/KPSS tests
Results: From 1999 to 2023, the age-adjusted mortality rate (AAMR) for aortic aneurysm and dissection in the U.S. declined markedly from 15.88 to 6.6 per 100,000. ARIMA modeling forecasted an AAMR of 6.32 (95% CI: 5.90–6.79) in 2025 and 5.48 (95% CI: 4.92–6.19) in 2030, with good model fit (RMSE = 0.450; Ljung-Box p = 0.242). Joinpoint regression identified the most rapid decline between 2006 and 2009 (Annual Percent Change [APC] = –10.78), coinciding with the widespread adoption of endovascular aneurysm repair (EVAR), despite its initially delayed adoption into clinical practice. Urban–rural disparities were evident, with the most significant decline observed in large central metro areas (AAMR: 14.52 to 5.16) compared to non-core rural areas (18.25 to 7.38). Regionally, the Midwest had the highest mortality in 1999 and experienced the steepest decline over time. Racial disparities persisted, with White individuals accounting for the highest number of deaths but also demonstrating the most pronounced decline (AAMR: 16.5 to 6.12; APC = –5.35). Non-Hispanic males had the highest mortality rates overall (AAMR: 24.55 to 8.39; AAPC = –4.61), while Hispanic females consistently had the lowest.
Conclusions: From 1999 to 2023, mortality from aortic aneurysm and dissection declined significantly, driven by advances such as endovascular aneurysm repair (EVAR) and improved clinical care. However, notable disparities by race, sex, and region remain despite these advances, highlighting the need for patient-centered selection, ongoing outcome reevaluation, and an equitable approach to care delivery.
More abstracts on this topic:
A Case Report: Outpatient Diagnosis of Venous Stent Migration - Avoiding Catastrophic Outcomes
Basnyat Anouksha, Pamganamamula Madhu, Naidu Raja, Pamganamamula Teja, Manchiraju Srinidhi, Gaddam Srilakshmi, Panganamamula Lalitha
A Meta-Analysis of Prospective Studies Comparing Short and Longterm Outcomes of Trans-Catheter Aortic Valve Replacement in Patient with and without Cancer:Khan Muhammad Aslam, Haider Adnan, Haider Taimoor, Bhattarai Shraddha, Khan Bilal, Lamichhane Bikal, Shafique Nouman, Rahman Hammad, Aafreen Asna, Muhammad Anza, Bhatia Hitesh, Khan Abid Nawaz Khan, Akbar Usman, Khan Alamzaib