Final ID: 4146824
Performance of Clinician-Assigned SCAI Shock Staging in the AHA Cardiogenic Shock Registry
Abstract Body (Do not enter title and authors here): Background: SCAI staging of cardiogenic shock (CS) severity facilitates communication about the presentation and trajectory of CS. Most prior validations of SCAI staging have used registry-specific algorithmic adaptations of the staging criteria. Few studies have evaluated clinician-assigned SCAI staging based on holistic assessment of all clinical data.
Aim: To assess the ability of initial and serial clinician-assigned SCAI staging to stratify risk of in-hospital mortality in a large, broadly representative CS population from the AHA CS Registry.
Methods: Consecutive CS admissions enrolled in the Registry (64 sites, 2022-2024) were included. Clinician-assigned SCAI stage was captured at CS onset (first 6h) and serially (6-12h after CS onset). Cases with available SCAI stage at both timepoints were classified as having improved, unchanged, or worsened SCAI stage. Associations of in-hospital mortality with initial and early change in SCAI stage were assessed using logistic regression; for the latter, models were adjusted for initial SCAI stage. Key subgroups defined by CS etiology (AMI-CS vs. HF-CS) and preceding cardiac arrest (CA) were examined.
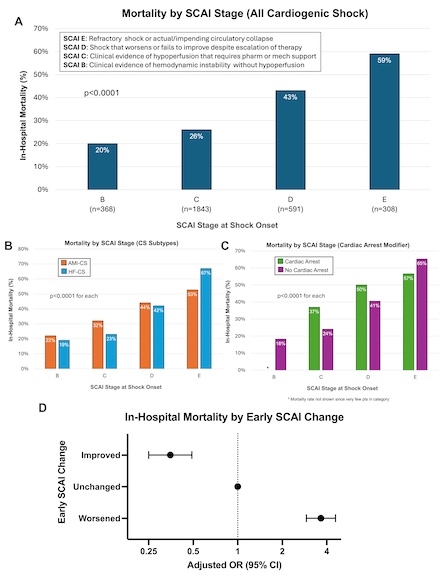
Results: Among 4,311 CS admissions, 3,110 (72%) had initial SCAI stage assessments (median age 66y, 33% women, 30% AMI-CS, 50% HF-CS, 21% preceding CA) and 2,867 (67%) had serial assessments. Most CS was initially staged as SCAI C (B: 12%; C: 59%; D: 19%; E: 10%), with a higher proportion of SCAI D/E in those with AMI-CS (34%) or preceding CA (60%). There was a stepwise gradient of mortality across SCAI stages (p<0.001; Fig-A), consistent when stratifying by CS etiology and preceding CA (p<0.001 for each; Fig-B/C). In the 12h after CS onset, most SCAI staging was unchanged (73%; worsening: 15%; improving: 12%); however, SCAI staging was more dynamic in those with preceding CA. Early worsening or improvement in SCAI stage was associated with higher (aOR 3.7, 95% CI 2.9-4.6) and lower (aOR 0.4, 95% CI 0.3-0.5) odds of mortality, respectively (Fig-D).
Conclusion: In this initial analysis from the AHA CS Registry, clinician-assigned SCAI staging effectively stratified in-hospital mortality risk, and early changes in SCAI stage further refined prognostication in CS.
Aim: To assess the ability of initial and serial clinician-assigned SCAI staging to stratify risk of in-hospital mortality in a large, broadly representative CS population from the AHA CS Registry.
Methods: Consecutive CS admissions enrolled in the Registry (64 sites, 2022-2024) were included. Clinician-assigned SCAI stage was captured at CS onset (first 6h) and serially (6-12h after CS onset). Cases with available SCAI stage at both timepoints were classified as having improved, unchanged, or worsened SCAI stage. Associations of in-hospital mortality with initial and early change in SCAI stage were assessed using logistic regression; for the latter, models were adjusted for initial SCAI stage. Key subgroups defined by CS etiology (AMI-CS vs. HF-CS) and preceding cardiac arrest (CA) were examined.
Results: Among 4,311 CS admissions, 3,110 (72%) had initial SCAI stage assessments (median age 66y, 33% women, 30% AMI-CS, 50% HF-CS, 21% preceding CA) and 2,867 (67%) had serial assessments. Most CS was initially staged as SCAI C (B: 12%; C: 59%; D: 19%; E: 10%), with a higher proportion of SCAI D/E in those with AMI-CS (34%) or preceding CA (60%). There was a stepwise gradient of mortality across SCAI stages (p<0.001; Fig-A), consistent when stratifying by CS etiology and preceding CA (p<0.001 for each; Fig-B/C). In the 12h after CS onset, most SCAI staging was unchanged (73%; worsening: 15%; improving: 12%); however, SCAI staging was more dynamic in those with preceding CA. Early worsening or improvement in SCAI stage was associated with higher (aOR 3.7, 95% CI 2.9-4.6) and lower (aOR 0.4, 95% CI 0.3-0.5) odds of mortality, respectively (Fig-D).
Conclusion: In this initial analysis from the AHA CS Registry, clinician-assigned SCAI staging effectively stratified in-hospital mortality risk, and early changes in SCAI stage further refined prognostication in CS.
More abstracts on this topic:
Adverse Events and Outcomes Among Patients with Temporary Mechanical Circulatory Support Devices Placed at Referring Versus Hub Cardiogenic Shock Centers
Patel Zachary, Silkowski Molly, Dodson Kaylen, Bull Lindsey, Gregoski Mathew, Tedford Ryan, Mcmurray Jeffrey, Witer Lucas, Kilic Arman, Houston Brian, Carnicelli Anthony, Ospina Meg, Mittelstaedt Roxanne, Peller Jacob, Samani Stephanie, Marchell Charlotte, Ohlrich Kelly, Gunn Brady, Varrone Michael
Adverse Events and Outcomes Among Patients with Temporary Mechanical Circulatory Support Devices Placed at Referring Versus Hub Cardiogenic Shock CentersPatel Zachary, Silkowski Molly, Dodson Kaylen, Bull Lindsey, Gregoski Mathew, Tedford Ryan, Mcmurray Jeffrey, Witer Lucas, Kilic Arman, Houston Brian, Carnicelli Anthony, Ospina Meg, Mittelstaedt Roxanne, Peller Jacob, Samani Stephanie, Marchell Charlotte, Ohlrich Kelly, Gunn Brady, Varrone Michael