Final ID: MP2163
Rising Burden of Hypertensive Emergency Hospitalizations in Young Adults: Insights from the National Inpatient Sample
Abstract Body (Do not enter title and authors here): Background: Hypertensive emergency burden in young adults is poorly characterized despite rising risk factors. We evaluated trends, characteristics, and mortality predictors in adults 18–49 hospitalized with hypertensive emergency.
Methods: We used the 2017–2019 NIS to identify hospitalizations with ICD-10 I16.1 in patients 18–49. Survey-weighted analyses yielded national estimates. Annual trends were examined overall and by age (18–29, 30–39, 40–49) and outcomes compared when hypertensive emergency was primary versus secondary. Logistic regression assessed mortality predictors including demographics, comorbidities, and hospital factors. Sensitivity analyses of I16.0, I16.9, and essential hypertension trends addressed coding artifacts.
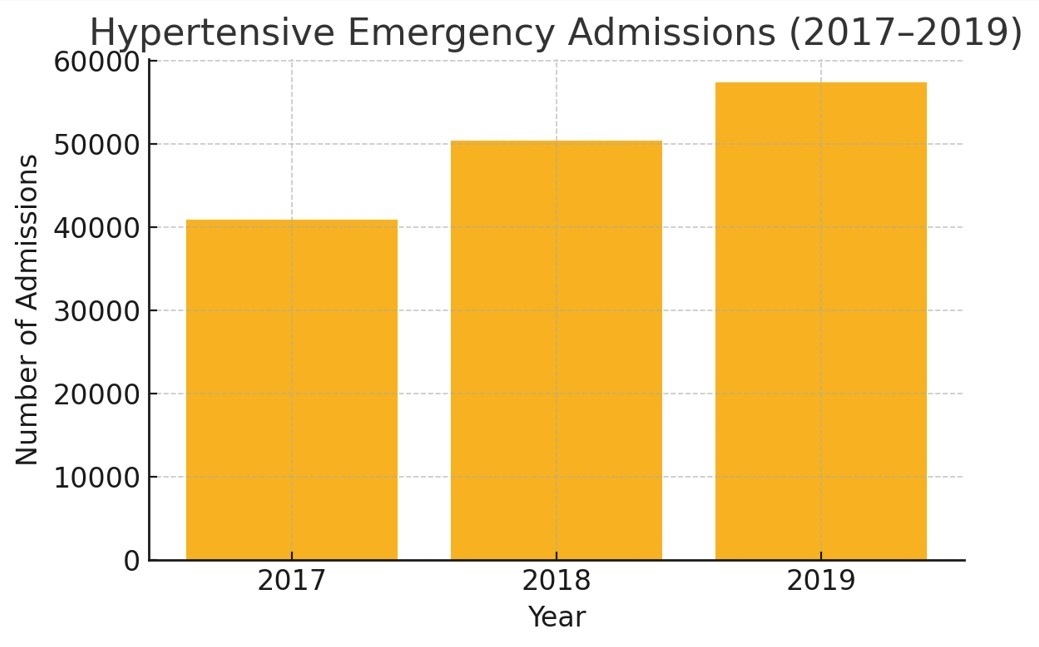
Results: From 29,711 unweighted hospitalizations, we estimated 148,555 hypertensive emergency admissions (2017–2019). Annual admissions rose from 40,835 to 57,335 (40.4% increase; p<0.001), most in 30–39 (44.7%) and 40–49 (42.6%) versus 18–29 (18.0%). All hypertensive crisis codes rose 24.9% while essential hypertension admissions fell 4.8%, indicating a true rise. Hypertensive emergency was primary in 34.1%. Mean age was 39.9 years; 56.8% male; racial distribution was 50.7% Black, 26.8% White, 13.6% Hispanic, and 3.1% Asian/Pacific Islander. In-hospital mortality was 1.56%, markedly lower when primary (0.16%) versus secondary (2.28%; 14-fold difference; p<0.001). Primary diagnosis predicted lower mortality (OR 0.12; 95% CI 0.06–0.24; p<0.001). Each year of age increased risk (OR 1.04; 95% CI 1.02–1.07; p=0.001). Black race was linked to lower mortality versus White (OR 0.65; 95% CI 0.44–0.96; p=0.03) despite younger age (39.7 vs 40.5 years) and higher primary diagnosis proportion (36.7% vs 32.2%).
Conclusions: Young adult hypertensive emergency hospitalizations rose 40% (2017–2019), especially ages 30–49. The 14-fold mortality disparity between primary and secondary diagnoses suggests distinct phenotypes—acute crisis versus complication. Paradoxical lower mortality in Black patients—despite higher acuity—warrants further study. These findings underscore a growing public health crisis necessitating prevention and early intervention.
Methods: We used the 2017–2019 NIS to identify hospitalizations with ICD-10 I16.1 in patients 18–49. Survey-weighted analyses yielded national estimates. Annual trends were examined overall and by age (18–29, 30–39, 40–49) and outcomes compared when hypertensive emergency was primary versus secondary. Logistic regression assessed mortality predictors including demographics, comorbidities, and hospital factors. Sensitivity analyses of I16.0, I16.9, and essential hypertension trends addressed coding artifacts.
Results: From 29,711 unweighted hospitalizations, we estimated 148,555 hypertensive emergency admissions (2017–2019). Annual admissions rose from 40,835 to 57,335 (40.4% increase; p<0.001), most in 30–39 (44.7%) and 40–49 (42.6%) versus 18–29 (18.0%). All hypertensive crisis codes rose 24.9% while essential hypertension admissions fell 4.8%, indicating a true rise. Hypertensive emergency was primary in 34.1%. Mean age was 39.9 years; 56.8% male; racial distribution was 50.7% Black, 26.8% White, 13.6% Hispanic, and 3.1% Asian/Pacific Islander. In-hospital mortality was 1.56%, markedly lower when primary (0.16%) versus secondary (2.28%; 14-fold difference; p<0.001). Primary diagnosis predicted lower mortality (OR 0.12; 95% CI 0.06–0.24; p<0.001). Each year of age increased risk (OR 1.04; 95% CI 1.02–1.07; p=0.001). Black race was linked to lower mortality versus White (OR 0.65; 95% CI 0.44–0.96; p=0.03) despite younger age (39.7 vs 40.5 years) and higher primary diagnosis proportion (36.7% vs 32.2%).
Conclusions: Young adult hypertensive emergency hospitalizations rose 40% (2017–2019), especially ages 30–49. The 14-fold mortality disparity between primary and secondary diagnoses suggests distinct phenotypes—acute crisis versus complication. Paradoxical lower mortality in Black patients—despite higher acuity—warrants further study. These findings underscore a growing public health crisis necessitating prevention and early intervention.
More abstracts on this topic:
A machine learning model for individualized risk prediction of ischemic heart disease in people with hypertension in Thailand
A Longitudinal 20-year Analysis Indicates Acceleration of Cardiometabolic Comorbidities on Dementia Risk
Sakboonyarat Boonsub, Poovieng Jaturon, Rangsin Ram
A Longitudinal 20-year Analysis Indicates Acceleration of Cardiometabolic Comorbidities on Dementia Risk
Lihua Huang, Danish Muhammad, Auyeung Tw, Jenny Lee, Kwok Timothy, Abrigo Jill, Wei Yingying, Lo Cecilia, Fung Erik