Final ID: MP2034
Prognostic Impact of Baseline Frailty, Malnutrition, or Both on Mortality for Patients Admitted with Acute Decompensated Heart Failure
Abstract Body (Do not enter title and authors here): Introduction: Malnutrition and frailty are highly prevalent among heart failure (HF) patients and have been shown to independently affect outcomes. However, these diagnoses are often overlooked during an acute decompensate HF (ADHF) hospitalization. In this retrospective analysis, we use data from a large, cardiac focused health system to assess the prognostic impact of baseline frailty and/or malnutrition on all-cause mortality at 30 days, 90 days, and 1 year following an ADHF hospitalization.
Hypothesis: Baseline frailty and/or malnutrition will confer a higher mortality risk in patients admitted for ADHF.
Methods: All Icahn Mount Sinai Health System patients were searched using TriNetX from 1/1/2005 through 4/30/2025. Patients aged >18 years with pre-existing HF admitted for ADHF were included. Patients who did not meet the inclusion criteria or who died during the index event were excluded. The control HF cohort was composed of included patients who did not have either malnutrition or frailty. The cohorts were propensity matched and balanced for baseline characteristics (i.e. BMI, age, sex, etc.). Statistical analysis was performed via Cox regression using the built-in TriNetX calculator. Outcomes are reported as hazard ratios (HR) with 95% confidence intervals (CI).
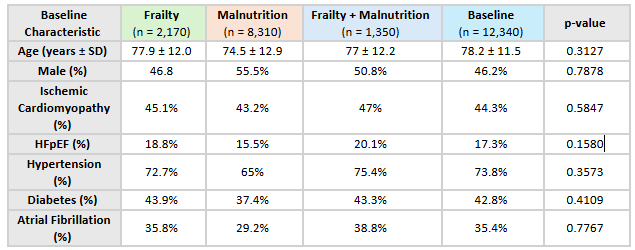
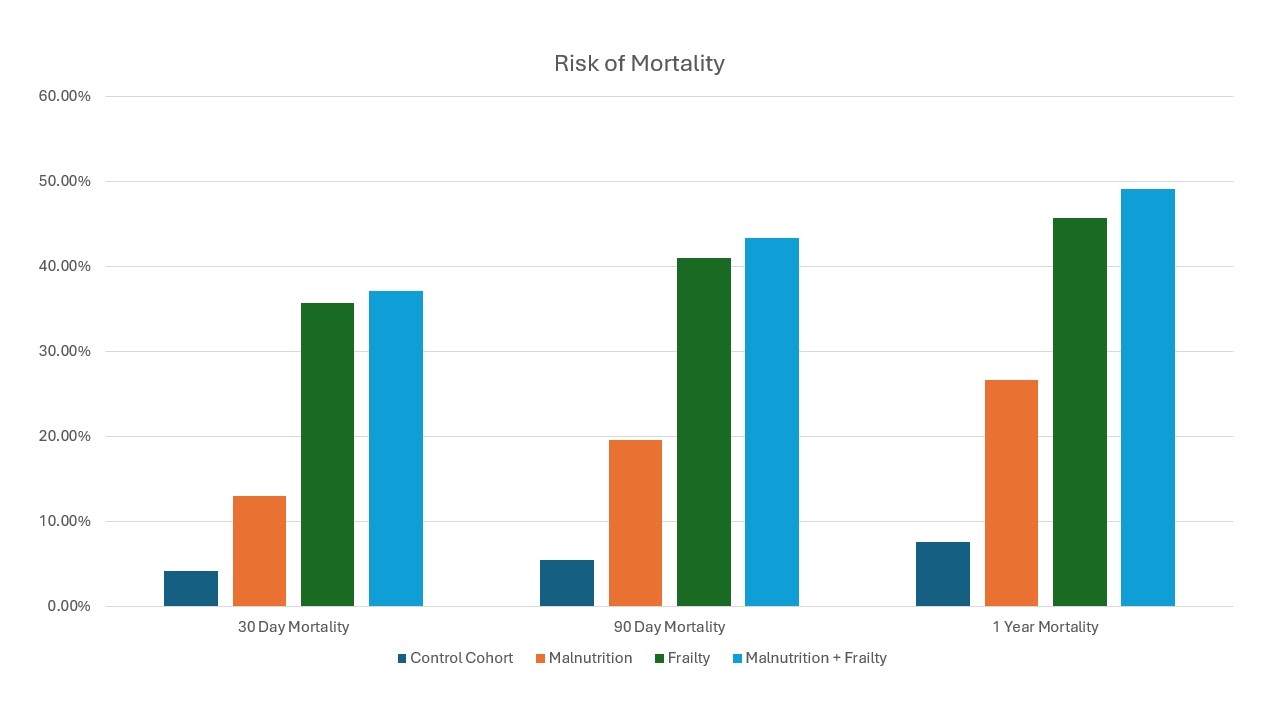
Results: A total of 24,860 patients admitted for ADHF were included (Frailty n=2,770; malnutrition n=8,310; frailty + malnutrition n=1,350; control HF n=12,340). Baseline characteristics of the cohorts are reported in Table 1. There was a significant increase in the risk of all-cause mortality at 30 days, 90 days, and 1 year post-discharge seen with baseline frailty (30 days: HR 6.423 95% CI 5.487-7.518 p<0.0001, 90 days: HR 5.783 95% CI 5.037-6.339 p=0.0002, 1 year: HR 4.856 95% CI 4.312-5.648 p<0.0001), malnutrition (30 days: HR 3.231 95% CI 2.861-3.65 p<0.0001, 90 days: HR 1.612 95% CI 1.345 - 1.933 p<0.001, 1 year: HR 3.947 95% CI 3.617-4.308 p<0.0001), or both (30 days: HR 9.826 95% CI 7.538-12.808 p<0.0001, 90 days: HR 8.638 95% CI 6.91-10.799 p=0.0349, 1 year: HR 8.036 95% CI 6.612-9.766 p<0.001). (Figure 1)
Conclusion: Frailty and malnutrition are significant independent risk factors for mortality post-discharge for ADHF, with as high as a 9-fold increased risk when both are present. Future prospective studies looking at early assessment and interventions for ADHF patients with frailty and malnutrition are needed to address this vulnerable population with high morbidity and mortality.
Hypothesis: Baseline frailty and/or malnutrition will confer a higher mortality risk in patients admitted for ADHF.
Methods: All Icahn Mount Sinai Health System patients were searched using TriNetX from 1/1/2005 through 4/30/2025. Patients aged >18 years with pre-existing HF admitted for ADHF were included. Patients who did not meet the inclusion criteria or who died during the index event were excluded. The control HF cohort was composed of included patients who did not have either malnutrition or frailty. The cohorts were propensity matched and balanced for baseline characteristics (i.e. BMI, age, sex, etc.). Statistical analysis was performed via Cox regression using the built-in TriNetX calculator. Outcomes are reported as hazard ratios (HR) with 95% confidence intervals (CI).
Results: A total of 24,860 patients admitted for ADHF were included (Frailty n=2,770; malnutrition n=8,310; frailty + malnutrition n=1,350; control HF n=12,340). Baseline characteristics of the cohorts are reported in Table 1. There was a significant increase in the risk of all-cause mortality at 30 days, 90 days, and 1 year post-discharge seen with baseline frailty (30 days: HR 6.423 95% CI 5.487-7.518 p<0.0001, 90 days: HR 5.783 95% CI 5.037-6.339 p=0.0002, 1 year: HR 4.856 95% CI 4.312-5.648 p<0.0001), malnutrition (30 days: HR 3.231 95% CI 2.861-3.65 p<0.0001, 90 days: HR 1.612 95% CI 1.345 - 1.933 p<0.001, 1 year: HR 3.947 95% CI 3.617-4.308 p<0.0001), or both (30 days: HR 9.826 95% CI 7.538-12.808 p<0.0001, 90 days: HR 8.638 95% CI 6.91-10.799 p=0.0349, 1 year: HR 8.036 95% CI 6.612-9.766 p<0.001). (Figure 1)
Conclusion: Frailty and malnutrition are significant independent risk factors for mortality post-discharge for ADHF, with as high as a 9-fold increased risk when both are present. Future prospective studies looking at early assessment and interventions for ADHF patients with frailty and malnutrition are needed to address this vulnerable population with high morbidity and mortality.
More abstracts on this topic:
Associations of Dietary Zinc Intake with Cardiovascular Disease and Mortality: Results from the Prospective Urban and Rural Epidemiology (PURE-China) Study
Li Xiaocong, Cai Qiujing, Huang Yilin, Biyan Biyan, Li Wei
5-oxoproline/ OPLAH Axis Alleviates Doxorubicin-induced Cardiomyopathy By Inhibiting FerroptosisJiang Meng, Guo Xinning