Final ID: MP1220
Cangrelor Versus Oral P2Y12 Inhibitors During PCI in Cardiogenic Shock and Cardiac Arrest: A Systematic Review and Meta-analysis
Abstract Body (Do not enter title and authors here): Background: Patients with cardiogenic shock or out-of-hospital cardiac arrest undergoing percutaneous coronary intervention face delayed absorption of oral P2Y12 inhibitors due to impaired gastrointestinal perfusion, increasing thrombotic risk. Cangrelor, an intravenous P2Y12 inhibitor with immediate onset, may offer clinical benefit in these critically ill populations. We performed a systematic review and meta-analysis to evaluate the safety and efficacy of cangrelor compared with oral P2Y12 inhibitors in this setting.
Research Question: Does cangrelor improve clinical outcomes compared with oral P2Y12 inhibitors in patients undergoing PCI for cardiogenic shock or cardiac arrest?
Methods: We searched PubMed and Embase through May 1, 2025, for observational studies comparing cangrelor and oral P2Y12 inhibitors in patients with cardiogenic shock or out-of-hospital cardiac arrest undergoing PCI. Outcomes included all-cause mortality, major bleeding, stent thrombosis, and stroke. Risk ratios (RR) with 95% confidence intervals (CI) were pooled using a random-effects model. Heterogeneity was assessed using the Chi-squared test and I2 statistic. Subgroup analysis was performed based on clinical presentation.
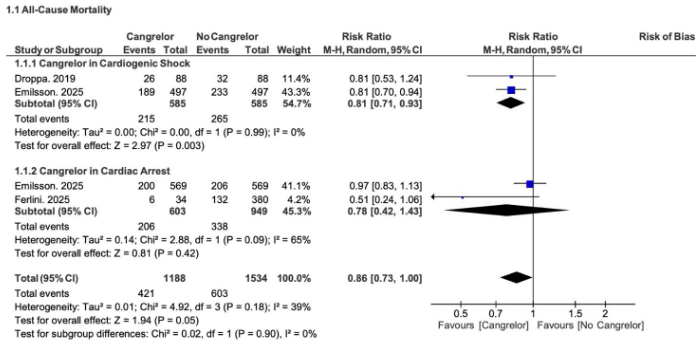
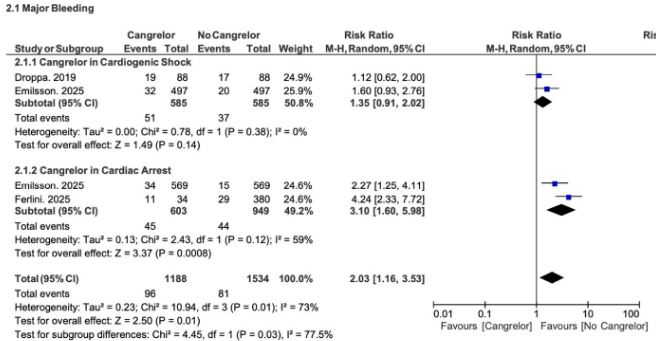
Results: Four studies, including 2,722 patients (1,170 with cardiogenic shock; 1,552 with out-of-hospital cardiac arrest) were analyzed. In cardiogenic shock, cangrelor significantly reduced mortality (RR: 0.81; 95% CI: 0.71–0.93; p = 0.003) without increasing major bleeding (RR: 1.35; 95% CI: 0.91–2.02). In cardiac arrest, cangrelor did not significantly reduce mortality (RR: 0.78; 95% CI: 0.42–1.43) and was associated with increased bleeding risk (RR: 3.10; 95% CI: 1.60–5.98; p = 0.0008). No significant differences were observed for stroke or stent thrombosis.
Conclusion: Cangrelor use during PCI in cardiogenic shock was associated with lower mortality and no excess bleeding, supporting its use in this high-risk group. However, in out-of-hospital cardiac arrest, the increased risk of bleeding warrants caution. These findings suggest a phenotype-specific approach to antiplatelet therapy in patients undergoing PCI under critical conditions.
Research Question: Does cangrelor improve clinical outcomes compared with oral P2Y12 inhibitors in patients undergoing PCI for cardiogenic shock or cardiac arrest?
Methods: We searched PubMed and Embase through May 1, 2025, for observational studies comparing cangrelor and oral P2Y12 inhibitors in patients with cardiogenic shock or out-of-hospital cardiac arrest undergoing PCI. Outcomes included all-cause mortality, major bleeding, stent thrombosis, and stroke. Risk ratios (RR) with 95% confidence intervals (CI) were pooled using a random-effects model. Heterogeneity was assessed using the Chi-squared test and I2 statistic. Subgroup analysis was performed based on clinical presentation.
Results: Four studies, including 2,722 patients (1,170 with cardiogenic shock; 1,552 with out-of-hospital cardiac arrest) were analyzed. In cardiogenic shock, cangrelor significantly reduced mortality (RR: 0.81; 95% CI: 0.71–0.93; p = 0.003) without increasing major bleeding (RR: 1.35; 95% CI: 0.91–2.02). In cardiac arrest, cangrelor did not significantly reduce mortality (RR: 0.78; 95% CI: 0.42–1.43) and was associated with increased bleeding risk (RR: 3.10; 95% CI: 1.60–5.98; p = 0.0008). No significant differences were observed for stroke or stent thrombosis.
Conclusion: Cangrelor use during PCI in cardiogenic shock was associated with lower mortality and no excess bleeding, supporting its use in this high-risk group. However, in out-of-hospital cardiac arrest, the increased risk of bleeding warrants caution. These findings suggest a phenotype-specific approach to antiplatelet therapy in patients undergoing PCI under critical conditions.
More abstracts on this topic:
Association Between Hospital Teaching Status and Outcomes in Patients with Cardiogenic Shock Complicating Acute Myocardial Infarction
Arshad Muhammad Sameer, Iqbal Naeem, Kumari Komal, Manal Ishba, Nasir Aamna, Javaid Syed Sarmad, Arshad Anosha, Abbas Faizan, Abideen Zain Ul, Fatima Saba, Harrison Marian, Hassan Shahzaib, Irshad Ayman
A Hospital-Wide Multidimensional Approach to Pediatric In-Hospital Cardiac Arrest Review: Early Identification and PreventionLoeb Daniel, Collins Kelly, Ortega Karina, Dewan Maya