Final ID: MP290
Does invasive hemodynamic monitoring reduce mortality? A Meta-Analysis of pulmonary artery catheterization in cardiogenic shock
Abstract Body (Do not enter title and authors here): Introduction
Cardiogenic shock is a life-threatening complication of decompensated heart failure, with elevated in-hospital mortality rates despite advances in treatment. Pulmonary artery catheterization (PAC) provides detailed hemodynamic data that may guide therapy in shock states, yet its routine use has declined following neutral trials in broader heart failure populations. The benefit of PAC in patients with cardiogenic shock remains uncertain.
Research question
In patients with cardiogenic shock, does the use of pulmonary artery catheter compared to standard therapy reduce in-hospital mortality?
Methods
We conducted a systematic review and meta-analysis including both observational studies and randomized controlled trials that compared the use of PAC versus no PAC in patients with cardiogenic shock. A comprehensive search was carried out in PubMed, Scopus, Cochrane CENTRAL, and Web of Science databases. Data were pooled using a random-effects model, and the certainty of the evidence was assessed using the GRADE approach. Primary outcomes included mortality, while secondary outcomes were length of hospital stay and procedure-related complications.
Results
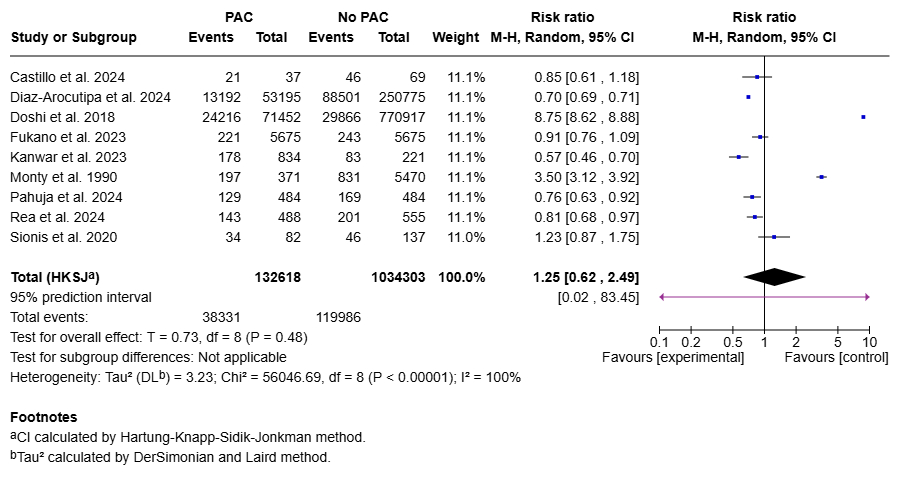
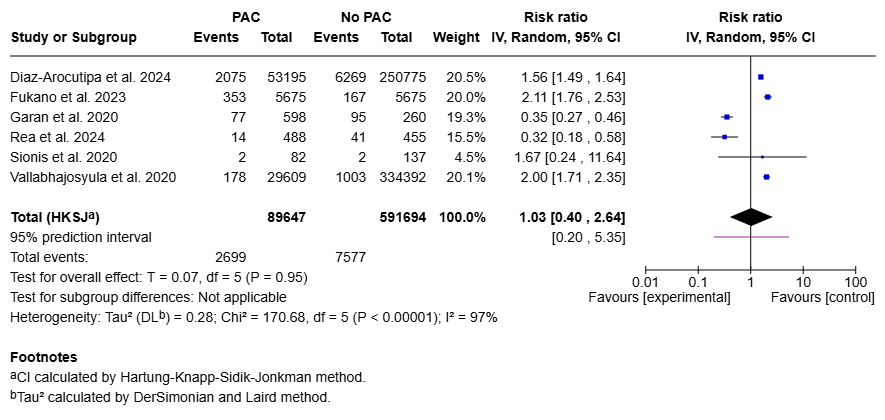
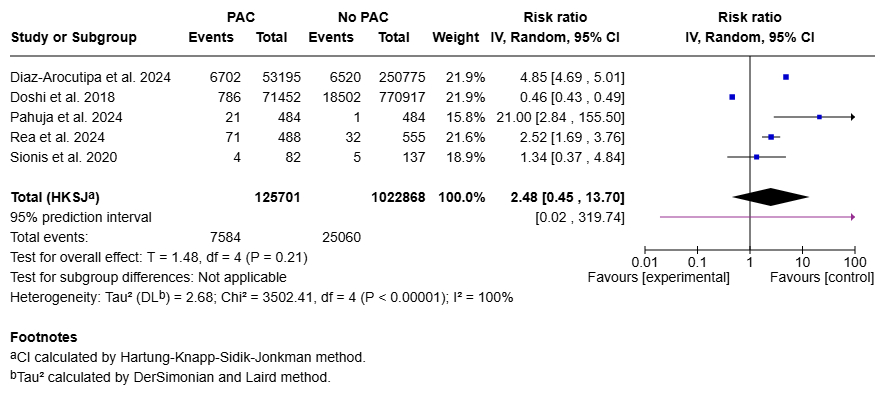
Nine studies including over 1.1 million patients with cardiogenic shock were analyzed. PAC was not associated with reduced in-hospital mortality compared to no PAC (RR 1.25, 95% CI 0.62–2.49; p=0.48). No significant differences were found in the use of vasoactive agents (RR 1.12, 95% CI 0.94–1.34; p=0.13), renal replacement therapy (RR 1.06, 95% CI 0.25–4.53; p=0.90), intra-aortic balloon pump (RR 2.00, 95% CI 0.84–4.73; p=0.09), ECMO (RR 1.03, 95% CI 0.40–2.64; p=0.95), or durable ventricular assist device implantation (RR 2.48, 95% CI 0.45–13.70; p=0.21). All outcomes showed high heterogeneity and wide prediction intervals, indicating substantial variability and uncertainty in treatment effects across studies.
Conclusion
PAC was not associated with significant benefits in mortality or major clinical endpoints. These findings suggest that PAC use should be individualized, and highlight the need for prospective trials to better define which patients may derive benefit from invasive hemodynamic monitoring.
Cardiogenic shock is a life-threatening complication of decompensated heart failure, with elevated in-hospital mortality rates despite advances in treatment. Pulmonary artery catheterization (PAC) provides detailed hemodynamic data that may guide therapy in shock states, yet its routine use has declined following neutral trials in broader heart failure populations. The benefit of PAC in patients with cardiogenic shock remains uncertain.
Research question
In patients with cardiogenic shock, does the use of pulmonary artery catheter compared to standard therapy reduce in-hospital mortality?
Methods
We conducted a systematic review and meta-analysis including both observational studies and randomized controlled trials that compared the use of PAC versus no PAC in patients with cardiogenic shock. A comprehensive search was carried out in PubMed, Scopus, Cochrane CENTRAL, and Web of Science databases. Data were pooled using a random-effects model, and the certainty of the evidence was assessed using the GRADE approach. Primary outcomes included mortality, while secondary outcomes were length of hospital stay and procedure-related complications.
Results
Nine studies including over 1.1 million patients with cardiogenic shock were analyzed. PAC was not associated with reduced in-hospital mortality compared to no PAC (RR 1.25, 95% CI 0.62–2.49; p=0.48). No significant differences were found in the use of vasoactive agents (RR 1.12, 95% CI 0.94–1.34; p=0.13), renal replacement therapy (RR 1.06, 95% CI 0.25–4.53; p=0.90), intra-aortic balloon pump (RR 2.00, 95% CI 0.84–4.73; p=0.09), ECMO (RR 1.03, 95% CI 0.40–2.64; p=0.95), or durable ventricular assist device implantation (RR 2.48, 95% CI 0.45–13.70; p=0.21). All outcomes showed high heterogeneity and wide prediction intervals, indicating substantial variability and uncertainty in treatment effects across studies.
Conclusion
PAC was not associated with significant benefits in mortality or major clinical endpoints. These findings suggest that PAC use should be individualized, and highlight the need for prospective trials to better define which patients may derive benefit from invasive hemodynamic monitoring.
More abstracts on this topic:
A Cross-scale Causal Machine Learning Framework Pinpoints Mgl2+ Macrophage Orchestrators of Balanced Arterial Growth
Han Jonghyeuk, Kong Dasom, Schwarz Erica, Takaesu Felipe, Humphrey Jay, Park Hyun-ji, Davis Michael E
Acute Right Ventricular Systolic Dysfunction Diagnosed by Transesophageal Echocardiography in Patients Post-Cardiac Arrest and Undifferentiated Shock: The Role of Clot in Transit DetectionDieiev Vladyslav, Salinas Pedro